Artificial intelligence, chatbots and ChatGPT in healthcare—narrative review of historical evolution, current application, and change management approach to increase adoption
Introduction
Artificial intelligence (AI), a field of study that combines computer science and robust datasets, continues to attract attention from clinicians, healthcare professionals, and researchers globally. When used appropriately in patient care and administrative processes in healthcare settings, AI has the potential to transform the process of healthcare delivery by making predictions based on available data. Numerous studies have shown that AI can be used for diagnosis, problem solving, identification of key disease features, and treatment planning process for complex clinical cases. For example, data from the American Cancer Society indicates that a high percentage of mammograms yield false results and patients often receive incorrect information, however incorporation of AI in diagnostic procedures leads to a more accurate diagnosis (99% accurate) eliminating the need for unnecessary biopsies and procedures (1). AI tools can also be used in detecting complex diseases such as malignant tumors and helping clinical researchers to plan trials and other research activities (2).
In modern medicine, AI has been significantly used to support clinical decision making and analysis of images collected during diagnostic and treatment planning process. AI provides clinicians with quick access to relevant research studies/clinical trials and assists them in making evidence-based decisions about different diseases/problems faced by patients (such as treatment options or therapy). In imaging, AI tools help to examine scans, X-rays, magnetic resonance imaging, and pictures of lesions or other details a radiologist may miss or overlook while diagnosing a problem (3). The coronavirus disease 2019 (COVID-19) pandemic has proven to be a catalyst, allowing researchers and innovative thinkers to design solutions that would enable clinicians to examine patients and provide care without coming in direct contact with patients (3).
This article focuses on detailed examination of the history and evolution of AI including chatbots and ChatGPT in healthcare. This is followed by a detailed Strengths, Weaknesses, Opportunities, Threats (SWOT) analysis of AI and associated tools that could lead to better patient experiences and enhanced health outcomes. Additionally, change management approach utilizing Kotter’s 8-Step process provides a roadmap for clinicians and healthcare leaders to integrate these tools in their practice and decision making at both clinical and administrative levels have been presented. With more than a decade of experience in academics, research, and healthcare industry, authors of this manuscript have provided recommendations for healthcare practitioners and leaders who are interested in implementing these tools and employing AI at large within their healthcare organizations.
Background
It has been projected that AI and its tools have the potential to create an impact on the lives of clinicians, healthcare leaders, counselors, mental health professionals, and patients. The clinical AI algorithms, chatbot, and ChatGPT have the potential to improve processes in different fields such as discovery of new drugs; research and clinical trials; diagnosis and treatment in radiology, surgery, oncology, and dermatology. AI technology has changed how retail and financial business sectors conduct business leading to considerable profits and improvement in their practices. If AI technology were to have a similar impact on healthcare, then this discipline can help in improving lives of millions of people (4). Recent data suggests that healthcare spending still account for over 18% of the gross domestic product (more than 4 trillion USD) (4,5). Overtreatment, inability to provide appropriate care to patients, and “subpar vigilance delivery” are some of the reasons behind increasing costs/expenditure. As stated previously, AI-based systems can drastically reduce such inefficiencies, leading to substantially more efficient and cost-effective health ecosystem (5). There is enough evidence that demonstrates AI has the ability or even surpass work accomplished by experts in fields such as image-based diagnosis particularly in pneumonia, dermatological classification of skin lesions, detection of lymph nodes metastases in cases of breast cancer, and diagnosis of heart ailments (6-10). Prior research projects conducted in South Asia, India, and USA have clearly shown that automated AI algorithms can be successfully utilized in diabetic retinopathy leading to better patient outcomes and increased cost savings. This was also demonstrated by the approval of AI algorithm “IDx-DR” by the Center for Medicare and Medicaid Services (CMS) in recent years (11). Recent studies in the field of radiotherapy and cancer treatment show that AI-based technology can significantly decrease preparation time for certain type of cancers (particularly head-neck and prostrate) thereby reducing wait times for life saving treatment (12,13).
Despite the publicity and possibilities there has been minimal AI adoption in healthcare (4). The barriers to adoption include but are not limited to algorithmic and data access limitations, regulations, too much reliance on data, and limited or no time to conduct research while dealing with (and taking care of) human lives at the same time. Because one must continuously examine problems with a network generated algorithm, there is an increased risk that AI will lead to solutions that are flawed or not correct. It must be noted that lack of transparency leads to decline in trust on AI (and tools of AI) and reduction in usage by healthcare practitioners. Furthermore, limited access to information, not having the time to conduct research in clinical settings, and arduous data collection process that can adversely impact patient flow creates barriers to adoption (4).
Working on research, data collection process, and access to information is extremely difficult in healthcare settings as these processes may result in disruption of workflow in patient care processes. It is also hard to collaborate and gather data across hospitals or different healthcare organizations/systems. To make clinical decisions, practitioners should have access to large, high quality data sets through AI enabled processes. Inability to compile large data sets creates issues in adoption of technology. The problem of slow adoption is compounded by the highly regulated nature of healthcare, liability concerns, privacy issues, and arduous approval process for the new technology (4).
In every field including healthcare, change is never easy and comes with questions. Approximately 50% of all organizational change can be unsuccessful (14). There is a need to conduct studies to examine historical evolution and effectiveness of AI tools and how healthcare practitioners and leaders can work on implementing such tools to provide better healthcare and treatment options to patients. Implementing AI into practice would result in a transformational change for healthcare (14). To successfully implement this change, leaders could utilize a theoretical model of change, such as Kotter’s 8-Step Change process. This process aligns with the steps of leading a transformational change by following eight critical steps when leading change: (I) create a sense of urgency; (II) build a guiding coalition; (III) develop and form a vision and strategy; (IV) enlist a volunteer army by communicating the change vision; (V) enable action by removing barriers and empowering broad-based change; (VI) generate short-term wins; (VII) sustain acceleration, consolidate gains, produce more change; and (VIII) institute change by anchoring new approaches in the culture (15,16). This framework will be further explored and applied to AI implementation steps later in the paper.
Rationale
There is dearth of research that examines history, evolution, and how healthcare organizations can effectively integrate tools of AI in their daily clinical work and healthcare leadership practices. As the field of AI and machine learning continues to evolve, it is even more important to understand historical perspective, previously completed work, and different methodologies that would allow us to successfully implement tools of AI in healthcare practice. These tools can be used in clinical decision making, research trials, patient engagement, and even providing contact less care to patients (up to a certain level), which is even more important considering recent changes brought upon us by the COVID-19 pandemic. This can also help hospital-based organizations, senior support facilities, policy makers, government officials, and researchers as they work on exploring innovative tools to streamline current practices in healthcare organizations.
Significance
As noted above, there is still a paucity of work in the rapidly evolving field of AI and as it applies to the field of healthcare (both clinical and administrative procedures). This work can be of value to leaders, researchers, and clinicians who wish to incorporate AI in their practice and future work. Publication of findings and dissemination through various channels could help hospitals, skilled nursing facilities, academic institutions, and other organizations who wish to utilize technology tools in their work. Inclusion of these tools in clinical care delivery and administrative practices can lead to high quality, safe, efficient, and timely care to patients. This may also result in cost savings for healthcare providers.
Objectives of the study
The objectives of the study:
- To examine history, evolution, and development of AI, chatbots, and ChatGPT;
- To conduct SWOT of AI (including chatbots and ChatGPT) in healthcare;
- To offer solutions and recommendations for implementation and success of AI, chatbots, and ChatGPT in healthcare organizations using a change management process.
We present this article in accordance with the Narrative Review reporting checklist (available at https://jmai.amegroups.com/article/view/10.21037/jmai-23-92/rc).
Methods
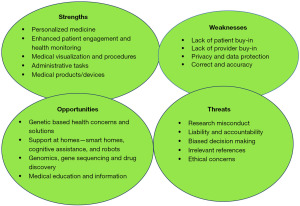
This descriptive study examines history of AI, chatbots, and ChatGPT and explores methods/approach how clinicians and healthcare leaders can include these tools to enhance healthcare delivery and improve quality, safety, and efficiency of healthcare services provided to patients. An initial literature search on history of AI, AI in healthcare, chatbots and ChatGPT was completed to examine and identify relevant manuscripts previously published. Table 1 presents summary of the adopted search strategy. A SWOT analysis has been completed to understand opportunities and strengths of the rapidly growing field of AI in healthcare. SWOT analysis helps in identification and examination of weaknesses and opportunities in the healthcare environment. This tool can be utilized by leaders, researchers, and clinicians when leading change initiatives in adopting and implementing AI into practice. It should be noted that this methodology is appropriate as it allows us to identify and understand means/assets and how organizations can utilize these tools to enhance effectiveness of healthcare delivery. Additionally, thorough analysis of external threats and opportunities allows healthcare practitioners to carefully plan their approach while integrating these tools in day-to-day practices. Researchers have completed a systematic analysis for the collected evidence. This evidence is comprised of scholarly manuscripts/articles, published thesis, government websites and reports, scholarly search engines, and other resources available to authors of this study.
Table 1
| Items | Specification |
|---|---|
| Date of search | February 1, 2023, and September 15, 2023 |
| Database | Google Scholar, PubMed, and Scopus |
| Search terms | Chatbot in healthcare, chatbot in hospitals, ChatGPT, healthcare technology, Artificial Intelligence, history of AI, history of chatbot and ChatGPT |
| Time frame | 2012–2023 |
| Inclusion/exclusion criteria | Inclusion: manuscripts in English language. Manuscripts in other languages were not considered |
| Selection process | AS under the direction of J.S. and B.S. |
AI, artificial intelligence.
Results
History of AI, chatbots, and ChatGPT
1950–1970
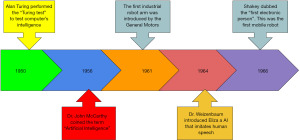
The time between 1950–1970 is marked by the birth of field of AI and technology behind it allowing researchers/innovators to further experiment, research, and develop a new and powerful tool that has the potential to have a meaningful impact on healthcare system, political climate, and our society as a whole (demonstrated in Figure 1). Dr. Alan M. Turing, a British mathematician who is widely known in the field of AI, was the first to describe that a computer can be used to simulate human behavior and thinking. In one of his contributions/book Computers and Intelligence, he proposed a test (later known as Turing Test) that would help us in determining whether computers are capable of thinking as a human. In 1956, Dr. John McCarthy, a legendary scientist coined the term “Artificial Intelligence” at a conference at Dartmouth College. He was one of the pioneers who paved the way for outstanding research in the field of AI, different branches of AI, and its application to different fields (17,18). As time progressed, we continued to witness major advancements in AI such as development of Unimate, the first robot arm at General Motors; creation of Eliza by Dr. Joseph Weizenbaum, a software that allowed users to converse with the computer programs as if they were interacting with a real person; and finally Shakey, the first robot, that was able to map the surroundings, work on problem solving tasks and understand commands given in plain simple English (18,19).
1970–2000
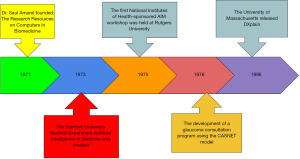
Majority of the period between 1970–2000 is portrayed as the “AI winter” primarily due to lack of activities resulting from scarcity of funding, declining interest, and increase in cost needed to support initial infrastructure required to build momentum for research and development activities. However, many researchers such as Dr. Saul Amarel, Professor of Computer Sciences at Rutgers University founded the Research Resource on Computers in Biomedicine in 1971. Two years later in 1973, Stanford University established a time-shared computer system to work collaboratively with clinical and biomedical researchers across different institutions. While there were conferences that were organized to support on-going development (such as first National Institute of Health AIM workshop), the development of glaucoma consultation program by utilizing the CASNET model can be seen as the first original example/model to show how AI can be applied to clinical practice. By incorporating model construction, consultation, and expert database, this program helped physicians by providing valuable patient care advice. This model was developed at Rutgers University and presented at the 1976 Academy of Ophthalmology meeting in the United States (18,20-22). Another key development in 1986, was the creation of DXplain, a decision support program. Originally designed by researchers at the University of Massachusetts, this program was used as an electronic medical textbook and helped physicians with differential diagnosis when information about patient symptoms were entered in the system. It should also be noted that this program included additional references and descriptions to help physicians reach a decision about diseases and treatment planning (18,22). Figure 2 demonstrates development that took place between 1970–2000.
2000–2023
As the field of AI continued to evolve, we saw major advancements such as being able to identify and analyze patterns across data sets, machine made decisions, data extraction from human language and decision making and sub-field of computer vision where machines were able to acquire information and understanding from images and videos. This created opportunities for a personalized approach towards medicine and patient care.
History of chatbots and ChatGPT
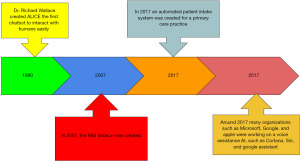
It is noteworthy that the history of chatbots and ChatGPT dates to around 1990’s when significant advancements were made in the field of AI. ALICE (Artificial Linguistic Internet Computer Entity), the first chatbot that was able to interact with human beings easily, was created by Richard Wallace at Massachusetts Institute of Technology (MIT) (23). This was followed by the development of Watson by IBM with the unique feature of being able to comprehend complex questions and provide answers like normal human interaction. Ten years later in 2017, Bakkar used Watson to detect and examine new RNA-binding protein that had undergone changes in a neurodegenerative disease. In the same year, Mandy, an automated patient intake system was also built for a primary care practice (18). With time, other organizations also made similar efforts which further led to the development of Cortana by Microsoft and Allo by Google. In 2017, the field of AI witnessed rapid growth with launch of Apple’s Siri and Chatfuel, a platform based on AI (23). This is demonstrated/shown in Figure 3.
Focused on its mission of ensuring benefits of AI to all humanity, Open AI, a research and deployment organization launched ChatGPT in 2022. Figure 4 traces the history of ChatGPT since 2016 when research on generative models was first published by OpenAI (24). These models function by utilizing existing data, images, and patterns to generate newer content. With additional research, further improvement in the Generative Pre-trained Transformer-2 (GPT-2) language model, enhanced functionality, lesser down time, being able to integrate ChatGPT in different web-based applications, and better reliability (24), one can expect that ChatGPT will be highly useful in various fields including the healthcare industry. Figure 4 summarizes the progression of ChatGPT.
SWOT analysis of application of AI, chatbots and ChatGPT in healthcare
A SWOT analysis was developed to help determine benefits and challenges with the current usage and future application of AI and chatbots including ChatGPT in healthcare industry (see Figure 5).
Strengths and opportunities
Precision medicine or personalized medicine allows healthcare professionals to design and consider treatment solutions based on the needs of individual patients while considering factors such as genetics, any underlying problems, demographic factors, and overall profile. By using complex algorithms, digital health applications, and “omics”-based tests, we can find innovative methods to help patients (25). By combining genetic information with AI algorithms, clinicians can draw correlations, examine different treatment options, and then consider possible outcome/prognosis as they plan effective care options for patients. Protein structure and expression, microbiome, and metabolic profile are utilized (in addition to genetic evidence) to plan treatment (25). With more than 10,000 participants in different parts of the world, Human Phenotype project is a leading example where data has been collected (and in-process) to identify molecular markers that can have significant impact on diagnosis, treatment planning, and prognosis of different diseases/health conditions. There is an effort to integrate AI to develop prediction models to monitor disease onset and progression (26).
AI enabled tools, chatbot and more specifically ChatGPT has been utilized to answer patients’ questions, help with decision making, and create a more structured approach while working with administrative processes such as patient scheduling and providing referrals (25). It should be noted clinicians and medical staff spend several hours every day on completing documents, checking electronic communication, and several other activities that can result in burnout and leads to waste of resources (27). Use of such AI tools could allow clinicians to focus their attention on patient care. Furthermore, these tools can help with communication as they are able to produce human like response to a variety of questions. For instance, one can incorporate the tools in remote patient monitoring, interpret and explain complex medical terminology which in turn allows patients to understand their medical problems, various treatment options available to them, and take more ownership of their health conditions (27).
Application and use of AI in genomics, gene sequencing, and process of drug discovery and design is growing at a very rapid pace. AI has already been widely used in clinical genomic analysis contributing to the overall accuracy of the process. One can expect that AI models will be extremely helpful in examining vast amounts of clinical and biomedical data which can accelerate further advancements in the field of genomic medicine leading to highly personalized care to patients (28).
Healthcare professionals and researchers have successfully applied AI to recognize patterns in imaging and provide in-depth examination of radiographic characteristics. In the field of radiation oncology, AI has been utilized in tumor delineation, examination, and assessment. It has also been widely used in radiomics with key benefits especially when clinicians need to process large number of images which leads to identification of disease characteristics that cannot be easily discerned by simple technology or naked eyes (14).
AI tools have been found to be extremely useful in minimally invasive surgery. It also holds the potential to significantly enhance the safety and efficacy of both robotic surgery and minimally invasive surgical procedures. With innovative and cutting-edge navigation and guidance mechanism, AI assists in improving the precision during surgery and medical procedures (29). More specifically, by identifying and tracking surgical instruments and body structures, image analysis can guide surgeons during complex procedures (30). Real time guidance during surgical process and education about use of technology can prevent complications or adverse events that may occur during the process (29).
Recently we have witnessed that there is an increased usage of AI and machine learning in hospitals, senior support facilities, and labs across the US. In 2022, the Food and Drug Administration (FDA) has approved more than 90 such devices that utilizes machine learning tools and/or algorithm (31). While initial approval has been primarily in the field of radiology or diagnostic medicine, strong collaboration between AI professionals, researchers, engineers, and clinicians will further lead to expansion and development in this rapidly evolving field of AI as it applies to medicine/healthcare (31).
Researchers have also indicated that AI (and associated technology) can be used to promote the concept of ambient assisted living, a means that would allow elderly to continue living in their home for a prolonged period. Smart homes equipped with different sensors, alarms, and tools that can conduct behavior analysis and assistive robots that can assist with different activities of daily living or robots such as RIBA that can help with lifting and moving things can help elderly/seniors at home. AI tools can also help with cognitive stimulation which results in better attention span, memory, and planning. This is particularly useful in the elderly who experience deterioration in cognitive abilities and face problems in completion of complex activities or tasks that require them to maintain attention and utilize problem solving skills (25).
The COVID-19 pandemic has encouraged innovators and researchers to consider care options that would incorporate AI-powered sensors and tools of technology to provide safe and high-quality care to patients without coming in direct contact with patients. For instance, Florida’s Tampa General Hospital installed an AI system to identify and separate people with potential COVID symptoms from other patients who visited the facility. By using cameras installed at entrances and technology that conducted facial thermal scans in addition to picking up on sweat and other symptoms, the hospital was able to curtail spread of the virus. Similar systems were put into place by other countries such as China and South Korea where AI-driven computed tomography (CT) scan interpreter, smart field hospitals, bracelet like devices, and robots were used to deliver medicines and food to patients (32). From this, health systems should carefully consider rapid and large-scale adoption of technology operated tools to provide care in the future (in case we are hit by another pandemic or natural disaster).
Widespread adoption of AI in healthcare can result in savings up to 10 percent in US healthcare on annual basis (up to $360 billion). These estimates are based on adoption of AI in healthcare processes without compromising quality or access to healthcare services. One can also expect better patient outcomes, increased satisfaction, high quality, and safer practices in healthcare settings (33).
A recently published report indicated that the US spends nearly $4 trillion on healthcare (34). It is noteworthy that administrative spending accounts for nearly one-quarter of the total spending. Administrative tasks that do not involve direct patient care take over half of nurses’ work and approximately 1/5 of physicians’ activities (35). AI can help with fraud detection/reduction, healthcare claims and billings, processes that involve communication from vast number of stakeholders, benefit management, electronic healthcare, and variety of other tasks that may lead to increased financial burden on organizations. Data suggests that Health Insurance Portability and Accountability Act (HIPAA) violations have resulted in loss of more than $75 million in last 7 years. This increases administrative burden on clinicians who now need to be aware of changing reimbursement methods/policies, new coding mechanisms, and other regulatory details to avoid any violations. AI can help by streamlining current processes and alleviating this burden on healthcare professionals (35).
Weakness and threats
Even though the field of AI is growing and will continue to expand, human surveillance is extremely important (10). Regulatory organizations, healthcare facilities, professional associations, and AI leaders must collaborate and establish systems to monitor progression of AI initiatives, patient safety initiatives, clinical risks, and any errors/adverse events (10,36). One cannot deny the importance of human input, review, and role of human practitioners even if facilities are equipped with surgery robots. Patients’ personal requirements play a critical role in care planning. AI system can identify a specific care center based on physical needs of patients; however, it should also be noted that social, economic, and other factors must be taken into consideration while allocating care. It is only possible to do so if healthcare providers are paying attention to personal needs of patients. Strict privacy laws, regulations, and compliance issues must be carefully considered when AI systems are incorporated (37). One cannot compare healthcare system to mobile phone company or organizations like Amazon, therefore access to information can pose challenges and limit AI’s ability to assist with medical practices. As noted above, while inclusion of AI may reduce cost and pressure on clinicians, it may also lead to elimination of certain jobs and pose equity challenges in current healthcare environment. A report published by the World Economic Forum indicated that incorporation of AI will lead to job losses and nearly 75 million jobs will be displaced particularly due to elimination of roles that entail repetitive tasks (37).
AI in medicine relies on diagnostic data available from vast number of clinical cases that are compiled over a period. In certain clinical cases or conditions where there is limited availability of data, one cannot ignore the possibility of misdiagnosis or missed diagnosis. Thus, human intervention and expertise is needed to help with complex or rare medical conditions (37). Inability for AI to help with diagnosis and treatment planning of certain conditions may lead to lack of buy in from both patients and providers.
Because AI systems rely on data network, they are also prone to security threats. It is important to consider possibilities of cyberattacks, along with other similar problems, and put appropriate safety mechanisms/procedures in place to ensure that patient data is protected (37). Benefits of application of AI in design and delivery of healthcare are widely acknowledged, but we should also examine ethical issues while using patient/clinical data. Four major issues that need to be addressed include: (I) informed consent for patients and providers to utilize data; (II) practices in place to ensure safety and transparency; (III) “algorithmic fairness” and bias issues; and (IV) privacy standards. Attention to these key factors/issues is needed to enforce implementation of transparent and equitable AI design. Lack of AI’s transparency is cited as one of the primary barriers to implementation in clinical and/or healthcare practices in general (38-40). The black-box problem/opacity on how AI reaches decisions is extremely important because patients’ health issues and lives are at stake (41,42). It is important to gain an understanding of how particular input has led to a specific output and different contributing factors that have led to a particular diagnosis. This is not always possible with AI and AI enabled systems. To build trustworthy AI systems which could lead to widespread adoption efforts should be made that organizations comply with laws and regulation, ethical practices and build secure and reliable system. A recent report by the European Institute of Innovation and Technology Health, recognized how “explainable, causal, and ethical AI” can help in adoption of such systems in practices (40,43). A governance model on how ethical challenges will be dealt with is also extremely important as we advance with widespread adoption of AI (44). This can be facilitated by the professional associations across the globe. More specifically, organizations such as the European Federation of Medical Informatics (45), International Medical Informatics Association, American Medical Informatics Association, and National Institute of Health Informatics can play a major role in dealing with ethical challenges noted above (46).
A recent article by Naik et al. [2022], indicated that “AI models can embed and deploy human and social biases at scale” (p.5). They also noted that models can be designed and prepared in such a way that it may reflect biases and inequities. Additionally, data collection methods (and way it is used) can also lead to bias, possibility of research misconduct, and addition of irrelevant references to the database which can be a challenge and issue especially when AI is utilized in clinical decision making. Future work should include new research, discussions, and steps to create and implement global governance models to guide researchers and clinicians as we move forward with adoption of AI in healthcare (44).
Discussion—challenges to adoption of AI, theoretical approach for adoption of AI & theoretical framework with recommendations
There is a growing need to consider adoption and implementation of AI tools into healthcare. AI would be considered a transformational change for the healthcare system. This change requires workers to redesign and adopt a new method of work. Resistance is a common result of any change but would be amplified when healthcare providers and workers are asked to adopt a new process of care delivery and processes (47). Due to this, leaders must consider utilizing a theoretical framework of change management. We suggest that Kotter’s 8-Step Change process could help facilitate the adoption and utilization of AI in healthcare. It must be noted that Kotter’s approach has been heavily utilized in business world (48), however there is still a dearth of studies that show that this methodology can be used in healthcare organizations (49). Kotter [2012] suggests that the methodology allow organizations to identify errors early in the process, detects faulty processes, and employees who are resistant to change initiatives. Because of highly systematic/structured nature of this approach, it is easily understandable by employees who may lead change initiatives in their respective departments/area of work within a complex setting such as healthcare organizations (50-53). Furthermore, reliance on data, ability to take feedback and make changes based on feedback, and celebration of small wins is a great advantage of Kotter’s approach which is particularly useful in healthcare environments (50,54). Kotter’s approach has been successfully applied in new diagnostic techniques (55), heart failure treatment (56), better outcomes for preterm newborns (57) and streamlining of communication processes in clinical care especially during shift handover (48,53,54).
Kotter’s 8-Step Change process is a widely recognized and utilized change management framework (47,51-53). The steps include: (I) establishing a sense of urgency; (II) creating a guiding coalition; (III) develop a vision and strategy; (IV) communicating the change vision; (V) empowering broad-based change; (VI) generating short-term wins; (VII) consolidating gains and producing more change; and (VIII) anchoring new approaches in culture. The benefit of this change management framework is that it approaches change in terms of operational and cultural aspects. Change requires a multi-faceted approach to ensure adoption of new processes. It is important to note there is no “one size fits all” approach to change management (47,51-53). Kotter’s 8-Step process can provide a guide for leaders to help implement change. The eight stages of Kotter are applied to AI adoption and outlined in the Table 2 below (47,51-53).
Table 2
| Stage | Application example |
|---|---|
| Establishing a sense of urgency | Rising healthcare costs require a new delivery of healthcare. A focus on detecting and diagnosing diseases earlier to format treatment plans are needed |
| Creating a guiding coalition | A group must be developed that can lead change. This group must be multidisciplinary and include leaders, providers, frontline staff, and patients |
| Develop a vision and strategy | The vision and strategy of AI should align and support the vision and strategy of the organization. The goal of AI adoption is to provide faster, more efficient, and less costly healthcare delivery by detecting, diagnosing, and forming a treatment plan. A focus will need to be placed on AI augmenting care delivery vs. replacing workers. Even though AI can replace human workers, we already know we have a deficit in healthcare workers, therefore AI could further support/assist vs. replace |
| Communicating the change vision | A common mistake by leaders is under-communicating change. Communication should center around the need for adopting AI to support faster, more efficient, and less costly healthcare. A key element in communication is the benefits of AI as assistive tool vs. replacement of human touch. In addition, leaders must be transparent about potential threats and weaknesses that may occur, such as cyberattacks, internet needs, and complexity of management of data sets |
| Empowering the broad-based change | Barriers must be removed related to adopting AI. Structural barriers around IT framework and adequate support need to be addressed with appropriate resources allocated. Provider, staff, and patient education must be developed and provided to answer questions and remove |
| Generating short-term wins | Any win should be celebrated. This helps build momentum. An example of a short-term win could be a pilot project with a group of patients in a radiology department related to detecting a specific disorder. Benefits to providers, staff, and the patient could be communicating across the healthcare system to help further validate the change direction and build further momentum to other areas in the system |
| Consolidating gains and producing more change | From pilot projects, leaders can help consolidate gains and continue to extend the utilization of AI across the system. The spread of this change will be dependent on the organizational resources and commitment to aligning AI into the vision of the organization. This step should ensure that AI starts to become an assistive tool throughout the system in terms of detection, diagnosis, assessment, and treatment planning |
| Anchoring new approaches in the culture | The goal is that AI becomes a new approach that is widely accepted in the organization. This step could take time as this follows a diffusion of innovation across the system. This can also be a time where staff and providers regress back if barriers and issues are encountered. Leaders must be at the ready to remove barriers and provide support. The vision and strategy need to be continued and communicated. Wins and examples must be shared to further support the widespread adoption of AI |
AI, artificial intelligence; IT, information technology.
We recommend that Kotter’s change could be an effective theoretical framework to support the implementation and adoption of AI including ChatGPT across a healthcare system (see Table 2). The framework provides systematic steps that leaders can utilize to infuse AI adoption throughout their organizations. It is important to identify that although these steps appear linear, the steps are interactive and earlier steps often need to be reinforced across the change time span (52). An important factor is having a committed change team with leadership during the implementation process (53). Communication, vision, and strategy needs to be provided throughout the implementation process. Leaders must secure resources and remove organizational barriers. We must celebrate any win and work to consolidate gains to continue the change momentum. The work of anchoring the changes in the culture does take time, so leaders must be willing to step back into previous stages of the process to continue to reinforce the adoption of AI tools into practice. AI should be considered by leaders to help augment clinical processes and workflows to create enhanced patient outcomes.
While Kotter’s change management approach can be utilized to support or lead implementation efforts, there needs to be careful consideration about ethical and regulatory aspects of AI usage/application in healthcare. Usage of incomplete or inadequate, under representative, and faulty datasets may lead to discrimination, lack of access to healthcare, and over/under estimation of risks in patient populations (58). Reducing or removing (ideal scenario) AI bias is extremely important for improved health outcomes. Faulty and poorly representative datasets lead to biases, incorrect estimates, medical errors, patient safety issues, and discrimination (59-61). We have seen that despite best efforts, some change initiatives fail to succeed (14). AI presents a potential solution of the health problems/challenges faced by healthcare organizations/systems globally. Efforts must be made to include training programs/education, clearly designed change management-based implementation strategy, and collaboration across hospitals, health systems, local and national government, and industry partnerships (62).
Limitations
This project relied on the existing literature, advances made in the field of AI, chatbots, and ChatGPT, and manuscripts/articles that were published primarily within last 10 years. However, authors did review manuscripts published 10 years ago (or more) while examining and tracing history and evaluation of AI and its usage in medicine and healthcare. While authors did conduct in-depth review of data available via different sources and utilized SWOT analysis and theoretical background that could help in rapid and widespread adoption of AI in healthcare, it should also be noted that findings may not be generalized across the globe. Given there are significant benefits resulting from adoption of AI, there is a clear need for further inquiry involving quantitative, qualitative, and mixed methods research procedures that could help create a better evidence-based system for clinical and administrative practices in healthcare settings.
Conclusions
AI combines computer science and robust datasets that could provide a new approach to patient and administrative processes in healthcare. AI has the potential to transform the process of healthcare delivery by making predictions based on data. As healthcare costs continue to rise, tools like chatbots and ChatGPT could augment existing care delivery in healthcare and result in more efficient and cost-effective processes. The utilization of AI tools could support assessment, diagnosis, and treatment planning. In addition, administrative workflows could be assessed and supported by AI tools.
To fully evaluate and implement AI utilization, leaders should understand the history of AI in healthcare. In addition, leaders should look at strengths, weaknesses, opportunities, and threats as they draft a change management plan for implementing and adopting AI. This paper provided a SWOT that could be adapted to an organization’s vision and strategy to assist them in adopting AI tools.
Leaders should utilize a theoretical change management process like Kotter’s 8-Step Change process when leading a transformational change. This process provides a systematic framework to help lead operational and cultural changes. We believe that AI should be considered by leaders to help augment clinical processes and workflows to create enhanced patient outcomes resulting in more efficient and cost-efficient healthcare. The future of healthcare depends on these assistive AI tools.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the Narrative Review reporting checklist. Available at https://jmai.amegroups.com/article/view/10.21037/jmai-23-92/rc
Peer Review File: Available at https://jmai.amegroups.com/article/view/10.21037/jmai-23-92/rc
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jmai.amegroups.com/article/view/10.21037/jmai-23-92/coif). B.S. voluntarily participated in the following boards: PioneerCare Board of Trustee, PioneerCare Corporation, Minnesota Organization of Leaders in Nursing, North Dakota Chapter of American College of Healthcare Executives, Member of Minnesota Organization of Leaders in Nursing, Member of American College of Healthcare Executives. No money or stipends are provided. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- PricewaterhouseCoopers. No longer science fiction, AI and robotics are transforming healthcare [Internet]. United States. Available online: https://www.pwc.com/gx/en/industries/healthcare/publications/ai-robotics-new-health/transforming-healthcare.html
- Davenport T, Kalakota R. The potential for artificial intelligence in healthcare. Future Healthc J 2019;6:94-8. [Crossref] [PubMed]
- International Business Machines Corporation. What is artificial intelligence in medicine. United States. Available online: https://www.ibm.com/topics/artificial-intelligence-medicine
- Goldfarb A, Teodoridis F. Why AI adoption in health care is lagging? Brookings, 2022. Available online: https://www.brookings.edu/articles/why-is-ai-adoption-in-health-care-lagging/
- Khanna NN, Maindarkar MA, Viswanathan V, et al. Economics of Artificial Intelligence in Healthcare: Diagnosis vs. Treatment. Healthcare (Basel) 2022;10:2493. [Crossref] [PubMed]
- Wang X, Peng Y, Lu L, et al. ChestX-Ray8: Hospital-Scale Chest X-Ray Database and Benchmarks on Weakly-Supervised Classification and Localization of Common Thorax Diseases. 2017 IEEE Conference on Computer Vision and Pattern Recognition (CVPR); 21-26 July 2017; Honolulu, HI, USA. IEEE; 2017:3462-71.
- Esteva A, Robicquet A, Ramsundar B, et al. A guide to deep learning in healthcare. Nat Med 2019;25:24-9. [Crossref] [PubMed]
- Ehteshami Bejnordi B, Veta M, Johannes van Diest P, et al. Diagnostic Assessment of Deep Learning Algorithms for Detection of Lymph Node Metastases in Women With Breast Cancer. JAMA 2017;318:2199-210. [Crossref] [PubMed]
- Strodthoff N, Strodthoff C. Detecting and interpreting myocardial infarction using fully convolutional neural networks. Physiol Meas 2019;40:015001. [Crossref] [PubMed]
- Bajwa J, Munir U, Nori A, et al. Artificial intelligence in healthcare: transforming the practice of medicine. Future Healthc J 2021;8:e188-94. [Crossref] [PubMed]
- Simonite T. The US government will pay doctors to use these AI algorithms. Wired, 2020. Available online: http://www.wired.com/story/us-government-pay-doctors-use-ai-algorithms
- Oktay O, Nanavati J, Schwaighofer A, et al. Evaluation of Deep Learning to Augment Image-Guided Radiotherapy for Head and Neck and Prostate Cancers. JAMA Netw Open 2020;3:e2027426. [Crossref] [PubMed]
- Alverez-Valle J, Moore GJ. Project InnerEye open-source deep learning toolkit: Democratizing medical imaging AI. Microsoft, 2020. Available online: http://www.microsoft.com/en-us/research/blog/project-innereye-open-source-deep-learning-toolkit-democratizing-medical-imaging-ai
- Bi WL, Hosny A, Schabath MB, et al. Artificial intelligence in cancer imaging: Clinical challenges and applications. CA Cancer J Clin 2019;69:127-57. [Crossref] [PubMed]
- Pakkasjärvi N, Luthra T, Anand S. Artificial intelligence in surgical learning. Surgeries 2023;4:86-97. [Crossref]
- Puliatti S, Eissa A, Checcucci E, et al. New imaging technologies for robotic kidney cancer surgery. Asian J Urol 2022;9:253-62. [Crossref] [PubMed]
- Stone P, Brooks R, Brynjolfsson E, et al. Artificial intelligence and life in 2030. One Hundred Year Study on Artificial Intelligence: Report of the 2015-2016 Study Panel, Stanford University, Stanford, CA. Available online: http://ai100.stanford.edu/2016-report
- Roboticsbiz. History of artificial intelligence in medicine. Available online: https://roboticsbiz.com/history-of-artificial-intelligence-in-medicine-aim/#google_vignette
- Szondy D. Fifty years of Shakey, the “world’s first electronic person”. Available online: https://newatlas.com/shakey-robot-sri-fiftieth-anniversary/37668/
- Kulikowski CA. Beginnings of Artificial Intelligence in Medicine (AIM): Computational Artifice Assisting Scientific Inquiry and Clinical Art - with Reflections on Present AIM Challenges. Yearb Med Inform 2019;28:249-56. [Crossref] [PubMed]
- Kulikowski CA. An Opening Chapter of the First Generation of Artificial Intelligence in Medicine: The First Rutgers AIM Workshop, June 1975. Yearb Med Inform 2015;10:227-33. [Crossref] [PubMed]
- Kumar R, Khan FU, Sharma A, et al. Recent Applications of Artificial Intelligence in the Detection of Gastrointestinal, Hepatic and Pancreatic Diseases. Curr Med Chem 2022;29:66-85. [Crossref] [PubMed]
- Digital Scholar. What is ChatGPT: The history of chatgpt – Open AI [2023]. Available online: https://digitalscholar.in/history-of-chatgpt/#the-history-of-chatgpt-its-predecessorshines
- Hines K. History of Chatgpt: A Timeline of the meteoric rise of generative AI chatbots. Search Engine Journal. Available online: https://www.searchenginejournal.com/history-of-chatgpt-timeline/488370/#close
- Bohr A, Memarzadeh K. The rise of artificial intelligence in healthcare applications. Artificial Intelligence in Healthcare 2020:25-60. doi:
10.1016/B978-0-12-818438-7.00002-2 .10.1016/B978-0-12-818438-7.00002-2 -
The Human Phenotype Project 2020 . Available online: https://mbzuai.ac.ae/the-node/ai-talks/ai-talk/the-human-phenotype-project/ - Siwicki B. Talkdesk talks about the benefits of being an early adopter of ChatGPT. Available online: https://www.healthcareitnews.com/news/talkdesk-talks-about-benefits-being-early-adopter-chatgpt
- Quazi S. Artificial intelligence and machine learning in precision and genomic medicine. Med Oncol 2022;39:120. [Crossref] [PubMed]
- Hashimoto DA, Rosman G, Rus D, et al. Artificial Intelligence in Surgery: Promises and Perils. Ann Surg 2018;268:70-6. [Crossref] [PubMed]
- Macek P, Cathelineau X, Barbe YP, et al. Robotic-Assisted Partial Nephrectomy: Techniques to Improve Clinical Outcomes. Curr Urol Rep 2021;22:51. [Crossref] [PubMed]
- Reuter E. 5 takeaways from the FDA’s list of AI-enabled medical device. MedTech Drive. 2022. Available online: https://www.medtechdive.com/news/FDA-AI-ML-medical-devices-5-takeaways/635908/
- Wittbold KA, Carroll C, Lansiti M, et al. How hospitals are using AI to battle COVID-19. Harvard Business Review.2020. Available online: https://hbr.org/2020/04/how-hospitals-are-using-ai-to-battle-covid-19
- Sanhi NR, Stein G, Zemmel R, et al. The potential impact of artificial intelligence on healthcare spending. United States: 2023 National Bureau of Economic Research, Inc.; 2023.
- CMS.gov. Historical. Available online: https://www.cms.gov/research-statistics-data-and-systems/statistics-trends-and-reports/nationalhealthexpenddata/nationalhealthaccountshistorical
- Sable M. Artificial intelligence for healthcare administration: A powerful tool for alleviating administrative burdens 2023. Available online: https://stratascale.com/artificial-intelligence-healthcare-administration-powerful-tool-alleviating-administrative-burdens
- Davahli MR, Karwowski W, Fiok K, et al. Controlling safety of artificial intelligence-based systems in healthcare. Symmetry 2021;13:102. [Crossref]
- Drexel University. Pros & cons of artificial intelligence in medicine. 2021. Available online: https://drexel.edu/cci/stories/artificial-intelligence-in-medicine-pros-and-cons/
- He J, Baxter SL, Xu J, et al. The practical implementation of artificial intelligence technologies in medicine. Nat Med 2019;25:30-6. [Crossref] [PubMed]
- Topol EJ. High-performance medicine: the convergence of human and artificial intelligence. Nat Med 2019;25:44-56. [Crossref] [PubMed]
- Markus AF, Kors JA, Rijnbeek PR. The role of explainability in creating trustworthy artificial intelligence for health care: A comprehensive survey of the terminology, design choices, and evaluation strategies. J Biomed Inform 2021;113:103655. [Crossref] [PubMed]
- Kiseleva A, Kotzinos D, De Hert P. Transparency of AI in Healthcare as a Multilayered System of Accountabilities: Between Legal Requirements and Technical Limitations. Front Artif Intell 2022;5:879603. [Crossref] [PubMed]
- Linardatos P, Papastefanopoulos V, Kotsiantis S, Explainable AI. A Review of Machine Learning Interpretability Methods. Entropy (Basel) 2020;23:18. [Crossref] [PubMed]
- European Institute of Innovation and Technology Health. Transforming healthcare with AI: The impact on the workforce and organisations. 2020. Available online: https://eithealth.eu/wp-content/uploads/2020/03/EIT-Health-and-McKinsey_Transforming-Healthcare-with-AI.pdf
- Naik N, Hameed BMZ, Shetty DK, et al. Legal and Ethical Consideration in Artificial Intelligence in Healthcare: Who Takes Responsibility? Front Surg 2022;9:862322. [Crossref] [PubMed]
- De Lusignan S, Barlow J, Scott PJ. Genesis of a UK Faculty of Clinical Informatics at a time of anticipation for some, and ruby, golden and diamond celebrations for others. J Innov Health Inform 2018;24:344-6. [Crossref] [PubMed]
-
American Medical Informatics Association n.d. ). Available online: https://amia.org/ - Mohiuddin S, Mohteshamuddin K. Combination model for sustainable change by utilizing Kotter’s change model and the Hersey & Blanchard leadership model for improving medication errors reporting. Journal of Medical and Allied Sciences 2020;10:25-32. [Crossref]
- Hospodková P, Berežná J, Barták M, et al. Change Management and Digital Innovations in Hospitals of Five European Countries. Healthcare (Basel) 2021;9:1508. [Crossref] [PubMed]
- Singh J, Singer AG, Paige A. Introducing change management education program for family medicine residents: a demonstration project. Can Med Educ J 2023;14:126-8. [Crossref] [PubMed]
- Miller, K. 5 critical steps in the change management process. 2020. Available online: https://online.hbs.edu/blog/post/change-management-process
- Kotter. The 8 steps to for leading change. Available online: https://www.kotterinc.com/methodology/8-steps/
- Pollack J, Pollack R. Using Kotter’s eight stage process to manage an organisational change program: Presentation and practice. Syst Pract Action Res 2014;28:51-66. [Crossref]
- Baloh J, Zhu X, Ward MM. Implementing team huddles in small rural hospitals: How does the Kotter model of change apply? J Nurs Manag 2018;26:571-8. [Crossref] [PubMed]
- Small A, Gist D, Souza D, et al. Using Kotter's Change Model for Implementing Bedside Handoff: A Quality Improvement Project. J Nurs Care Qual 2016;31:304-9. [Crossref] [PubMed]
- Maclean DF, Vannet N. Improving trauma imaging in Wales through Kotter's theory of change. Clin Radiol 2016;71:427-31. [Crossref] [PubMed]
- Dolansky MA, Hitch JA, Piña IL, et al. Improving heart failure disease management in skilled nursing facilities: lessons learned. Clin Nurs Res 2013;22:432-47. [Crossref] [PubMed]
- Ellsbury DL, Clark RH, Ursprung R, et al. A Multifaceted Approach to Improving Outcomes in the NICU: The Pediatrix 100 000 Babies Campaign. Pediatrics 2016;137:e20150389. [Crossref] [PubMed]
- Reddy S, Allan S, Coghlan S, et al. A governance model for the application of AI in health care. J Am Med Inform Assoc 2020;27:491-7. [Crossref] [PubMed]
- Whittlestone J, Nyrup R, Alexandrova A, et al. Ethical and societal implications of algorithms, data, and artificial intelligence: a roadmap for research. 2019. Available online: http://www.nuffieldfoundation.org/sites/default/files/files/Ethical-and-Societal-Implications-of-Data-and-AI-report-Nuffield-Foundat.pdf
- Cath C. Governing artificial intelligence: ethical, legal and technical opportunities and challenges. Philos Trans A Math Phys Eng Sci 2018;376:20180080. [Crossref] [PubMed]
- Cheatham B, Javanmardian K, Samandari H. Confronting the risks of artificial intelligence. McKinsey Quarterly. April 2019. Available online: https://www.mckinsey.com/business-functions/mckinsey-analytics/our-insights/confronting-the-risks-of-artificial-intelligence#
- Petersson L, Larsson I, Nygren JM, et al. Challenges to implementing artificial intelligence in healthcare: a qualitative interview study with healthcare leaders in Sweden. BMC Health Serv Res 2022;22:850. [Crossref] [PubMed]
Cite this article as: Singh J, Sillerud B, Singh A. Artificial intelligence, chatbots and ChatGPT in healthcare—narrative review of historical evolution, current application, and change management approach to increase adoption. J Med Artif Intell 2023;6:30.