Perceptions of the use and benefits of artificial intelligence applications: survey study
Highlight box
Key findings
• Artificial intelligence (AI) is easy to use and facilitates healthcare professionals in decision-making, increases efficiency, minimizes costs, performs the tasks with accuracy, and assists in informed decision-making. Secondly, AI integration, AI accuracy, and AI adoption by healthcare professionals have a positive and significant impact on patient outcomes.
What is known and what is new?
• AI is applied in all medical disciplines: radiology, dermatology, ophthalmology, cardiology, surgery and more. It improves medical knowledge through the exploitation of massive and complex data. AI helps improve patients’ quality of life. Many studies investigated the perceptions of AI among the health care employees.
• Few studies have examined the impact of the perception of ease of use, integration of AI in healthcare sector, accuracy and AI adoption, on patient outcomes. This work summarizes recent developments in AI in medicine, and provides the main use cases in which AI-powered medical technologies can be used. The aim of this study is to investigate the integration of AI in the healthcare system in Kingdom of Saudi Arabia, the perceived ease of use and usefulness of AI, to explore the integration of AI in healthcare sector, and to study the impact of AI accuracy and AI adoption by healthcare professionals on patient outcomes.
What is the implication, and what should change now?
• Researchers can develop AI models for disease prediction, risk factors specific to the Saudi population, and personalizing treatments. The integration of AI into genomics enables to understand the genetic variations specific to the Saudi population, for a more precise personalized medicine.
Introduction
Overview
Medicine is one of the fields in which Big Data is leading to the biggest changes, in the form of medical Big Data (MBD) (1). MBD, particularly when combined with artificial intelligence (AI), allows us to make faster progress (2). AI-powered medical technologies are rapidly evolving into applicable solutions for clinical practice. In a report published by the Swiss Medical Association, AI has the potential to improve the quality of medical care. It can both reduce human error and minimize doctors’ workload for routine tasks. It is useful for improvement in the following areas: Prevention, Diagnosis, Treatment, Patient monitoring, and repetitive administrative tasks (3). Despite the spectacular development of AI in recent years, the speed of its integration in medicine is not proportional to the speed of progress of the technology (4). In addition, AI applications still generate a lot of confusion and controversy about its potential benefits and risks, both among healthcare professionals and patients (5).
Related studies
The notion of AI has been present since antiquity (the golem in Jewish folklore, or Hephaestus in ancient Greek religion, who built automata and artificial creatures). But the first document on AI is the “intelligent machinery” presented by Alan Turing in 1948.
AI, or intelligent machine, can be described as a computerized system (AI system) able to make predictions and recommendations, and take decisions. In this way, it can influence real-life environments, with a human-defined objective (3). A sub-field of AI is machine learning, which teaches a computer to analyze large amounts of data quickly, using complex algorithms (6).
AI is already present in our daily lives. Familiar examples include Amazon’s product recommendation system for online shopping, ride-sharing apps like “Uber” or “Lyft”, intelligent personal assistants such as “Cortana”, “Alexa” and “Siri” (5), or “Florence”, the robot created by Amazon Web Services and Google Cloud, that develops a tobacco quit plan (7).
AI in medicine
In the past, some researchers, such as Lusted, have predicted that AI will eventually replace doctors in various fields (8). However, despite rapid technological advances, this has not occurred. AI has enabled a number of programs to be widely used in medicine (9). The medical community agrees that AI will have a radical impact on patient care in the near future (5).
According to the specialized literature, the impact of AI in medicine focuses on three areas: (I) the impact on healthcare systems (process improvement, minimization of medical errors, adaptation of healthcare, AI-based home monitoring combined with telemedicine); (II) impact on physicians (recognition systems, assisted decision-making, rapid and precise image interpretation); (III) the impact on patients: the possibility of tracking their data in order to promote their health.
AI is applied in all medical disciplines: radiology, pathology, dermatology, ophthalmology, cardiology, gastroenterology, psychiatry/psychotherapy, surgery and more. Even delicate microsurgical operations, such as intraocular procedures, can be performed with AI-assisted robotic systems (10).
Deep learning algorithms can deal with increasing amounts of data provided by wearables, smartphones and other mobile monitoring sensors in different areas of medicine (11). This will help in the precise diagnosis of diseases, the development of personalized treatments (12), the identification of public health trends and problems, as well as enabling individuals to take control of their health by accessing their health data and tracking their progress on an ongoing basis (1). Deep learning is used in particular to identify and interpret patterns found in medical imaging, pathological preparations, photographs of skin lesions or eye fundus, electrocardiograms or vital parameters (3).
A research, published in “Nature Medicine”, describes the effectiveness of AI for radiologists in detecting breast cancer in mammograms. More recently, a team of doctors has developed a symptom-based diagnosis that predicts a patient’s chances of contacting coronavirus disease 2019 (COVID-19) (13).
AI technologies applied in healthcare can profoundly transform medical practice and patient care. Many researchers believe that the most successful application area for medical AI is probably AI-assisted radiology image analysis (5,14,15).
AI techniques improve medical knowledge through the exploitation of massive and complex data (16). AI helps improve patients’ quality of life. For example, patients with cardiovascular disease (CVD) can receive cardiac rehabilitation (CR) at home, reducing the number of hospitalizations (17).
AI is also used in administration. In Switzerland, doctors working in acute somatic care devote up to 27% of their working time to documenting medical records (18). That’s why, in the USA, there are “clinical scribes” to draft documentation, reduce the administrative burden on doctors, and avoid the number of errors. Now, thanks to AI, there are “digital scribes” (19).
Perceptions of AI in healthcare sector
The Digital Trends Survey 2021 examined the perceptions of the medical community and the general population on the usefulness of digital healthcare applications. While doctors see the value of such applications, they are opposed to apps that are set to replace the doctor’s visit. The “human factor” is crucial to successful treatment. Almost all doctors surveyed refuse use intelligent applications for diagnosis (94%), or treatment planning (85%). The survey underlines that the main expectation from AI is to save doctors’ time and provide individualized care (20).
Many studies investigated the perceptions of AI among the health care employees. The study of Maskara et al. in 2017 among medical professionals in India shows that they are aware of AI interventions, and highlights some perceived disadvantages of AI (21). Oh et al. identified in 2019 positive attitudes among South Korean staff, who believe that roles will not be replaced by AI (22). Abdullah and Fakieh, in 2020, carry out a survey among health care employees in the Kingdom of Saudi Arabia (KSA), who have shown mixed attitudes and feelings regarding the implementation of AI technologies. Employees in the Saudi healthcare sector have a moderate level of acceptance of AI applications, with most respondents indicating concern that their jobs would be replaced by AI (23).
Zoom on AI in the KSA
The originality of this study is that it tests the relationships in the context of a country that is extremely interesting from the point of view of AI, and which is a pioneer in the Middle East and North Africa (MENA) region and Arab countries in general. Saudi Arabia also wants and has the resources to establish a unique position in the world on a global scale.
Following in the footsteps of several countries such as the USA and Europe, which aim to be pioneers in the field of AI, Saudi Arabia has taken several steps. As a reminder, in 2019 Trump signed the “Executive Order on Maintaining American Leadership in AI”, the White House launched “AI.gov”, and AI-related bills have been introduced in the US Congress. The European Commission is encouraging European Union (EU) members to develop a common AI strategy. The aim is to become the world-leading region for the development and application of “cutting-edge, ethical and secure AI” (24).
In this context, the KSA has taken far-reaching steps to take advantage of AI techniques in various fields, particularly after declaring the 2030 vision in which digitization is one of the main objectives. It is worth noting that the KSA is regarded as a technologically advanced country. Saudi Arabia’s internet penetration rate stood at 97.9% of the total population at the start of 2022 (25). Saudi Arabia has been among world’s top 10 in using Internet Protocol’s latest version (26). The kingdom ranks second globally in cybersecurity index according to World Competitiveness Yearbook 2022 (27). These numbers give the MENA region the fundamentals for AI application. The KSA is particularly well-positioned to become the regional AI powerhouse.
The KSA considers AI to be an important strategic tool for occupying a prominent place in the world. Major efforts are being made to develop AI in various fields, particularly in education and healthcare. The use of robots, innovative pharmacies and certain applications, such as TABAOD and TAWAKKALNA, are part of this approach (28). AI approaches improve disease recognition and treatment while personalizing patient care. For example, Alqahtani, in 2023, calls for action on CVD, which is the main cause of death in the kingdom, accounting for over 45% of all deaths. The development of CR programs is greatly facilitated by AI approaches and needs to be expanded (29).
Research questions
It is crucial to research the use of AI in healthcare in the KSA. We can find chances to enhance patient care and results by researching how AI is being used in healthcare in Saudi Arabia. Healthcare workers are in low supply in KSA, especially in rural regions. AI has the ability to close this gap by helping healthcare professionals with activities like patient monitoring and medical image interpretation, freeing them up to concentrate on more difficult ones. By lowering the need for hospital stays and pointless testing, as well as by optimizing resource allocation, the application of AI in healthcare may result in cost savings. This is crucial in Saudi Arabia, where growing healthcare expenses are a result of an aging population and a rise in chronic illnesses. Overall, research on AI in healthcare in Saudi Arabia has the potential to significantly advance patient care, workforce development, cost reductions, and policy choices. Effective communication and cooperation between management, healthcare workers, patients, and other stakeholders are necessary for this. This study aims to assess the impact of current AI Integration into the Healthcare System (AIHS) on Patient Outcomes (PQ) in KSA, to evaluate the impact of the accuracy of AI technology on healthcare outcomes in KSA, and to identify factors that facilitate or hinder AI adoption in healthcare in KSA.
To fill this gap, we have to answer the following questions:
- What is the impact of AIHS on PQ?
- How does the accuracy of AI technology impact PQ?
- How does the Adoption of AI Technology by Healthcare Professionals (AATHP) impact PQ?
The tested model is presented in Figure 1. We present this article in accordance with the SURGE reporting checklist (available at https://jmai.amegroups.com/article/view/10.21037/jmai-23-59/rc).
Methods
The present study employed a quantitative research methodology to thoroughly investigate the correlations, patterns, and consistencies among the sample population. The study employs descriptive statistics, including means, medians, modes, and standard deviations, to accurately depict the central tendency, variability, and distribution of their data. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). This study did not involve any experiment and thus the Institutional Review Board (IRB) approval is waived. Informed consent was taken from all individual participants.
Population and sample
The survey was conducted among a target population of 200 patients and healthcare professionals employed in four healthcare departments in Saudi Arabia. The establishment of this representative sample was purposeful and aimed to encompass a diverse spectrum of healthcare professionals and patients in the healthcare sector. The researcher employed already-established metrics to check the reliability and uniformity of the interrogatives. The survey was created using the Google Forms platform, which allowed for its online distribution and assisted in the gathering of a broad and representative sampling of the population.
Data analysis
The present study employed MS-Excel and Statistical Packages for the Social Sciences (IBM Corporation, New York, NY, USA) Version 21 and 27, respectively, to carry out the data analysis. In the initial phase of the analysis, demographic evaluation was performed utilizing pie charts and frequency and percentage analysis to scrutinize the personal data of the study’s participants. This study examines AI in Healthcare in KSA. In this research work, five major variables have been analyzed such as PEUU (Perceived Ease of Use and Usefulness); AIHS; AAT (Accuracy of the AI Technology); AATHP; PQ.
Results
Table 1 shows the distribution of demographic variables among the questionnaire sample. Most of the sample (76%) were male, as the majority of the sample were between 29 and 39 years old (60%). The majority of the respondents had a bachelor’s degree (62.5%). Moreover, nearly half of the respondents are employed in the public sector (53.5%). Also, almost half of the respondents have a monthly income higher than 15,000 Saudi Riyal (SAR). And finally, the majority of the respondents need less than one hour to get to the Health Facility they usually use.
Table 1
| Demographic and variable | Frequency, n (%) |
|---|---|
| Gender | |
| Male | 152 (76.0) |
| Female | 48 (24.0) |
| Age (years) | |
| 18–28 | 48 (24.0) |
| 29–39 | 120 (60.0) |
| 40–50 | 29 (14.5) |
| >50 | 3 (1.5) |
| Educational level | |
| High school | 7 (3.5) |
| Associate degree | 3 (1.5) |
| Bachelor’s degree | 125 (62.5) |
| Master’s degree or higher | 65 (32.5) |
| Employment status | |
| Employed in the private sector | 80 (40.0) |
| Employed in the public sector | 107 (53.5) |
| Self-employed | 1 (0.5) |
| Unemployed | 3 (1.5) |
| Other | 9 (4.5) |
| Monthly income | |
| Equal or less than 5,000 SAR | 9 (4.5) |
| 5,001–10,000 SAR | 18 (9.0) |
| 10,001–15,000 SAR | 55 (27.5) |
| More than 15,000 SAR | 106 (53.0) |
| Prefer not to say | 12 (6.0) |
| Time required to get to the health facility (hospital/clinic) the patient usually use | |
| Less than one hour | 135 (67.5) |
| One-two hours | 48 (24.0) |
| Two-three hours | 12 (6.0) |
| Three-four hours | 2 (1.0) |
| Four hours and more | 3 (1.5) |
SAR, Saudi Riyal.
Analysis of PEUU
Table 2 lists the respondents’ answers regarding PEUU of AI technologies in the healthcare sector.
Table 2
| Variable | Ease of use 1 | Ease of use 2 | Ease of use 3 | Ease of use 4 | Ease of use 5 | Ease of use 6 | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | % | N | % | N | % | N | % | N | % | N | % | ||||||
| Agree | 67 | 33.5 | 79 | 39.5 | 72 | 36 | 75 | 37.5 | 90 | 45 | 80 | 40 | |||||
| Disagree | 41 | 20.5 | 36 | 18 | 51 | 25.5 | 21 | 10.5 | 23 | 11.5 | 14 | 7 | |||||
| Neutral | 59 | 29.5 | 55 | 27.5 | 60 | 30 | 56 | 28 | 38 | 19 | 35 | 17.5 | |||||
| Strongly agree | 28 | 14 | 29 | 14.5 | 16 | 8 | 44 | 22 | 2 | 1 | 20 | 10 | |||||
| Strongly disagree | 5 | 2.5 | 1 | 0.5 | 1 | 0.5 | 4 | 2 | 47 | 23.5 | 51 | 25.5 | |||||
Table 2 shows that the majority of the respondents agrees, and strongly agrees, that AI is easy to use and functional and facilitates healthcare professionals in decision-making.
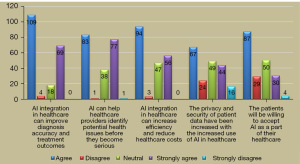
Analysis of AIHS
Table 3 lists the respondents’ answers regarding the integration of AI technologies into the healthcare system.
Table 3
| Variable | Diagnostic and treatment | Health issue identification | Reduce cost | Privacy and security | Patient acceptance | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | % | N | % | N | % | N | % | N | % | |||||
| Agree | 109 | 54.5 | 83 | 41.5 | 94 | 47 | 67 | 33.5 | 87 | 43.5 | ||||
| Disagree | 4 | 2 | 1 | 0.5 | 3 | 1.5 | 24 | 12 | 29 | 14.5 | ||||
| Neutral | 18 | 9 | 38 | 19 | 47 | 23.5 | 49 | 24.5 | 50 | 25 | ||||
| Strongly agree | 69 | 34.5 | 77 | 38.5 | 56 | 28 | 44 | 22 | 30 | 15 | ||||
| Strongly disagree | 0 | 0 | 1 | 0.5 | 0 | 0 | 16 | 8 | 4 | 2 | ||||
Figure 2 and Table 3 show that the majority of the respondents agree and strongly agree that AI integration in healthcare increases efficiency, and accuracy, minimizes costs, and enhances the treatment outcomes of the patients.
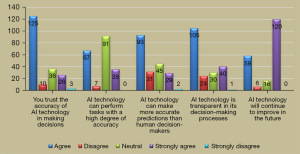
Analysis of the AAT
Table 4 lists the respondents’ answers regarding the accuracy of the AI technologies in the healthcare sector.
Table 4
| Variable | Trust | Accuracy | Accurate predictions | Transparency | Improvement of AI technology | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | % | N | % | N | % | N | % | N | % | |||||
| Agree | 125 | 62.5 | 67 | 33.5 | 93 | 46.5 | 105 | 52.5 | 58 | 29 | ||||
| Disagree | 10 | 5 | 7 | 3.5 | 31 | 15.5 | 24 | 12 | 6 | 3 | ||||
| Neutral | 36 | 18 | 91 | 45.5 | 45 | 22.5 | 30 | 15 | 16 | 8 | ||||
| Strongly agree | 26 | 13 | 35 | 17.5 | 29 | 14.5 | 40 | 20 | 120 | 60 | ||||
| Strongly disagree | 3 | 1.5 | 0 | 0 | 2 | 1 | 1 | 0.5 | 0 | 0 | ||||
Figure 3 and Table 4 show that the majority of the participants agree and strongly agree that the AI accurately predicts than the humans, performs the tasks with high accuracy, and assists in making informed decision making.
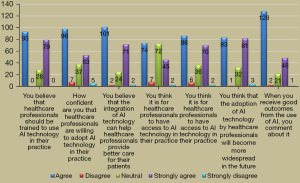
Analysis of the AATHP
Table 5 lists the respondents’ answers regarding the AATHP.
Table 5
| Variable | Training healthcare professionals | Willingness of healthcare professionals to adopt AI technology | Providing better care for patients | Access to AI technology | Widespread adoption of AI technology by healthcare professionals | Receiving good outcomes from the use of AI | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | % | N | % | N | % | N | % | N | % | N | % | ||||||
| Agree | 93 | 46.5 | 98 | 49 | 101 | 50.5 | 74 | 37 | 83 | 41.5 | 128 | 64 | |||||
| Disagree | 0 | 0 | 7 | 3.5 | 2 | 1 | 7 | 3.5 | 1 | 0.5 | 2 | 1 | |||||
| Neutral | 28 | 14 | 37 | 18.5 | 24 | 12 | 72 | 36 | 32 | 16 | 21 | 10.5 | |||||
| Strongly agree | 79 | 39.5 | 53 | 26.5 | 71 | 35.5 | 45 | 22.5 | 81 | 40.5 | 48 | 24 | |||||
| Strongly disagree | 0 | 0 | 5 | 2.5 | 2 | 1 | 2 | 1 | 3 | 1.5 | 1 | 0.5 | |||||
Figure 4 and Table 5 show that the majority of the participants agree and strongly agree that AI adoption in healthcare could provide better care, and the results also indicated that the majority of the participants believed that healthcare professionals should be trained to practice AI in the future for better healthcare outcomes.
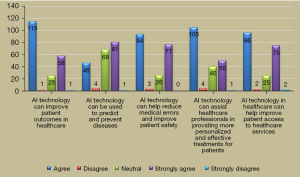
Analysis of the PQ
Table 6 lists the respondents’ answers regarding the PQ.
Table 6
| Variable | Improvement of patient outcomes | Use of technology to predict and prevent diseases | Reduction of medical errors and improvement of patient safety | Providing more personalized and effective treatments | Improvement of patient access to healthcare services | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | % | N | % | N | % | N | % | N | % | |||||
| Agree | 115 | 57.5 | 46 | 23 | 94 | 47 | 105 | 52.5 | 96 | 48 | ||||
| Disagree | 1 | 0.5 | 4 | 2 | 3 | 1.5 | 4 | 2 | 2 | 1 | ||||
| Neutral | 25 | 12.5 | 68 | 34 | 26 | 13 | 40 | 20 | 25 | 12.5 | ||||
| Strongly agree | 58 | 29 | 81 | 40.5 | 77 | 38.5 | 50 | 25 | 75 | 37.5 | ||||
| Strongly disagree | 1 | 0.5 | 1 | 0.5 | 0 | 0 | 1 | 0.5 | 2 | 1 | ||||
Figure 5 and Table 6 show that the majority of the participants agree and strongly agree that AI adoption and integration improves PQ by minimizing medical errors, improves access to healthcare, and assists healthcare professionals in predicting and preventing diseases.
Reliability analysis results
The results of the alpha in Table 7 suggest that all these variables are moving in the same direction and the highly related to each other. The value of reliability is greater than 0.7 which means that the data are internally reliable and consistent with each other. The five latent factors have been extracted by using the multivariate analysis technique in the form of factor analysis. The PEUU measured with the help of seven observed factors and the value of Kaiser-Meyer-Olkin (KMO) and Bartlett’s Test of Sphericity suggest that these seven variables are suitable to build latent variables of PEUU. On the other hand, AIHS has been extracted by using the five observed variables, and the values of the factor loading suggested that these variables have a higher level of association with the latent factor. The third latent factor of AAT is also measured by using the five observed variables, and higher factor loading shows the suitability of the observed variables to this latent factor. AATHP and PQ were also measured by using the seven and five observed variables, respectively.
Table 7
| Variable | Cronbach’s alpha | Cronbach’s alpha based on standardized items | N of items | Items | KMO | Bartlett’s Test of Sphericity |
|---|---|---|---|---|---|---|
| Perceived Ease of Use and Usefulness | 0.709 | 0.762 | 7 | PEUU-1 | 0.785 | <0.001 |
| PEUU-2 | ||||||
| PEUU-3 | ||||||
| PEUU-4 | ||||||
| PEUU-5 | ||||||
| PEUU-6 | ||||||
| PEUU-7 | ||||||
| AI Integration into the Healthcare System | 0.704 | 0.743 | 5 | AIHS-1 | 0.756 | <0.001 |
| AIHS-2 | ||||||
| AIHS-3 | ||||||
| AIHS-4 | ||||||
| AIHS-5 | ||||||
| Accuracy of the AI Technology | 0.736 | 0.757 | 5 | AAT-1 | 0.640 | <0.001 |
| AAT-2 | ||||||
| AAT-3 | ||||||
| AAT-4 | ||||||
| AAT-5 | ||||||
| Adoption of AI Technology by Healthcare Professionals | 0.795 | 0.797 | 7 | AATHP-1 | 0.799 | <0.001 |
| AATHP-2 | ||||||
| AATHP-3 | ||||||
| AATHP-4 | ||||||
| AATHP-5 | ||||||
| AATHP-6 | ||||||
| AATHP-7 | ||||||
| Patient Outcomes | 0.774 | 0.777 | 5 | PQ-1 | – | – |
| PQ-2 | ||||||
| PQ-3 | ||||||
| PQ-4 | ||||||
| PQ-5 |
KMO, Kaiser-Meyer-Olkin; AI, artificial intelligence; PEUU, Perceived Ease of Use and Usefulness; AIHS, AI Integration into the Healthcare System; AAT, Accuracy of the AI Technology; AATHP, Adoption of AI Technology by Healthcare Professionals; PQ, Patient Outcomes.
Model testing
The Pearson correlation test in Table 8 indicates that most of the variables are positively associated with each other at the 99% confidence level. The lower P value that shows that most variables are highly and significantly associated with each other. PEUU and AIHS have a higher degree and magnitude of the relationship, which further shows that these variables are moving in the same direction simultaneously because the value of correlation is greater than 0.7. AIHS enhances the PEUU. The AATHP improves PQ. The AAT and the PQ are also directly associated with each other, which indicates that the AAT improves the healthcare operations that are further directly associated with the outcomes of the patients. In short, PQ have a higher degree and magnitude of the relationship with all the explanatory variables at 99% and 95% confidence levels as far as the positive relationship is concerned.
Table 8
| Variable | Subtypes | PEUU | AIHS | AAT | AATHP | PQ |
|---|---|---|---|---|---|---|
| PEUU | Pearson correlation | 1 | 0.772** | 0.803** | 0.735** | 0.854** |
| Sig. (2-tailed) | 0.005 | <0.001 | 0.001 | 0.009 | ||
| N | 200 | 200 | 200 | 200 | 200 | |
| AIHS | Pearson correlation | 0.772** | 1 | 0.744** | 0.887** | 0.777** |
| Sig. (2-tailed) | 0.005 | 0.002 | 0.009 | <0.001 | ||
| N | 200 | 200 | 200 | 200 | 200 | |
| AAT | Pearson correlation | 0.803** | 0.744* | 1 | 0.789** | 0.810** |
| Sig. (2-tailed) | <0.001 | 0.042 | <0.001 | <0.001 | ||
| N | 200 | 200 | 200 | 200 | 200 | |
| AATHP | Pearson correlation | 0.735** | 0.887 | 0.789** | 1 | 0.665** |
| Sig. (2-tailed) | 0.001 | 0.219 | <0.001 | <0.001 | ||
| N | 200 | 200 | 200 | 200 | 200 | |
| PQ | Pearson correlation | 0.854** | 0.777** | 0.810** | 0.665** | 1 |
| Sig. (2-tailed) | <0.001 | <0.001 | <0.001 | <0.001 | ||
| N | 200 | 200 | 200 | 200 | 200 |
*, correlation is significant at the 0.05 level (2-tailed); **, correlation is significant at the 0.01 level (2-tailed). PEUU, Perceived Ease of Use and Usefulness; AIHS, AI Integration into the Healthcare System; AAT, Accuracy of the AI Technology; AATHP, Adoption of AI Technology by Healthcare Professionals; PQ, Patient Outcomes; AI, artificial intelligence.
The results of the analysis of variance (ANOVA) test in Table 9 show the overall significance of the model. The higher F value shows that there is a significant difference between the group means as far as the sample means are concerned. The P value of the Multivariate ANOVA is also second to the F value of the test. In other words, the model of the study has been fitted to the data and the sample size fully represents the population of all the variables. The variance samples are different for each variable, and overall, the model is a good fit at the 99% confidence level.
Table 9
| Model 1 | Sum of squares | df | Mean square | F | Sig. |
|---|---|---|---|---|---|
| Regression | 91.009 | 4 | 22.752 | 41.475 | <0.001 |
| Residual | 106.424 | 194 | 0.549 | ||
| Total | 197.433 | 198 |
ANOVA, analysis of variance.
According to Table 10, both the independent variables are directly positively associated with the dependent variable of firm performance. The value of the P of independent variables PEUU, AIHS, AAT, and AATHP is less than 0.05. It represents that the PEUU, AIHS, AAT, AATHP significantly and positively influences the PQ. AI integration in healthcare not only assists professionals in making more informed decisions but also increases the accuracy of health outcomes and minimizes medical errors in healthcare. Therefore, the results show that AI adoption and integration improve PQ.
Table 10
| Model 1 | Unstandardized coefficients | Standardized coefficients, beta | t | Sig. | Hypothesis | |
|---|---|---|---|---|---|---|
| B | Std. error | |||||
| (Constant) | 0.005 | 0.053 | 0.087 | 0.931 | ||
| PEUU | 0.133 | 0.057 | 0.133 | 20.519 | 0.021 | H1 |
| AIHS | 0.012 | 0.055 | 0.012 | 30.210 | 0.004 | H2 |
| AAT | 0.100 | 0.060 | 0.101 | 40.684 | 0.004 | H3 |
| AATHP | 0.656 | 0.058 | 0.658 | 110.345 | <0.001 | H4 |
PEUU, Perceived Ease of Use and Usefulness; AIHS, AI Integration into the Healthcare System; AAT, Accuracy of the AI Technology; AATHP, Adoption of AI Technology by Healthcare Professionals.
Discussion
Several examples of the influence of AI in medicine are presented. IBM’s Watson platform was developed from a massive database of millions of medical records, to help make accurate diagnoses and appropriate treatment plans. Watson advises on the best cancer treatments and performs genome analysis. Google’s DeepMind software is used to test automated classification of digital fundus photographs using optical coherence tomography. AI is also used to predict genetic variations in low-grade gliomas, identify genetic phenotypes in small-cell lung carcinoma, reduce false-positive rates in computer-assisted detection of screening mammograms, improve pathological detection of mediastinal lymph nodes and assess bone age (22).
Concerns about AI in medicine
Despite the benefits of AI, there are some fears. In the medical world, there are fears of doctors becoming dequalified (30). There are serious concerns about the safety of AI. A study carried out in the UK shows that 80% of respondents (doctors and other healthcare professionals) believe that the widespread use of AI could pose problems related to privacy. Forty percent agree with Elon Musk’s statement that “AI is more dangerous than nuclear weapons” (Musk, 2018) (5). Other concerns relate to the personal relationship between doctor and patient (3,31).
Principal findings
The majority of the respondents agrees, and strongly agrees, that AI is easy to use and functional and facilitates healthcare professionals in decision-making, that that AI integration in healthcare increases efficiency, and accuracy, minimizes costs, and enhances the treatment outcomes of the patients, and that the AI accurately predicts than the humans, performs the tasks with high accuracy, and assists in making informed decision making. There is also agreement among respondents that AI adoption in healthcare could provide better care, that healthcare professionals should be trained to practice AI in the future for better healthcare outcomes, and that AI adoption and integration improves PQ by minimizing medical errors, improves access to healthcare, and assists healthcare professionals in predicting and preventing diseases.
The results of the study show also that the PEUU has a positive and significant impact on the outcomes of the patients. Secondly, AIHS has a positive and significant impact on PQ. And, the accuracy of AI technology has a positive and significant impact on PQ. Finally, the AATHP has a positive and significant impact on the PQ.
Limitation
An important limitation is that the questionnaires were administered randomly between patients and healthcare professionals. This approach doesn’t capture the perceptions and attitudes of each segment separately. It would be interesting to examine the differences between these two groups independently.
Conclusions
This study assessed attitudes of medical staff and patients, toward AI implementation in the healthcare sector. The study was conducted in four hospitals in Riyadh, the capital of Saudi Arabia. The results showed that the population is extremely supportive and aware of the benefits of AI in the healthcare sector. this may be due to government efforts to invest in AI and make its use familiar to patients. Several AI apps have already been used for years in the KSA (SEHHATY, VEZEETA, TELADOC, PHARMALINE, TADAWI, etc.). Researchers can continue to develop AI models for disease prediction, identifying risk factors specific to the Saudi population, and personalizing treatments based on genetic and environmental characteristics. The integration of AI into genomics enables us to understand the genetic variations specific to the Saudi population and their impact on health. This can lead to better prediction of genetic disease risk and more precise personalized medicine. These are just a few examples of future research avenues in this revolutionary field.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the SURGE reporting checklist. Available at https://jmai.amegroups.com/article/view/10.21037/jmai-23-59/rc
Data Sharing Statement: Available at https://jmai.amegroups.com/article/view/10.21037/jmai-23-59/dss
Peer Review File: Available at https://jmai.amegroups.com/article/view/10.21037/jmai-23-59/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jmai.amegroups.com/article/view/10.21037/jmai-23-59/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). This study did not involve any experiment and thus the Institutional Review Board (IRB) approval is waived. Informed consent was taken from all individual participants.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Zhang Y, Hong J, Chen S. Medical Big Data and Artificial Intelligence for Healthcare. Appl Sci 2023;13:3745. [Crossref]
- Hulsen T, Petkovic M, Varga OE, et al. Editorial: AI in Healthcare: From Data to Intelligence. Front Artif Intell 2022;5:909391. [Crossref] [PubMed]
- L’intelligence artificielle dans le quotidien médical, Fédération des médecins suisses, Dr méd. Alexander Zimmer, membre du comité central de la FMH, responsable du département Numérisation /eHealth. Available online: https://www.fmh.ch/files/pdf27/20220914_fmh_brosch-ki_f.pdf
- Laï MC, Brian M, Mamzer MF. Perceptions of artificial intelligence in healthcare: findings from a qualitative survey study among actors in France. J Transl Med 2020;18:14. [Crossref] [PubMed]
- Castagno S, Khalifa M. Perceptions of Artificial Intelligence Among Healthcare Staff: A Qualitative Survey Study. Front Artif Intell 2020;3:578983. [Crossref] [PubMed]
- Shameer K, Johnson KW, Glicksberg BS, et al. Machine learning in cardiovascular medicine: are we there yet? Heart 2018;104:1156-64. [Crossref] [PubMed]
- Kaplan MS, Newsom JT, McFarland BH, et al. Demographic and psychosocial correlates of physical activity in late life. Am J Prev Med 2001;21:306-12. [Crossref] [PubMed]
- LUSTED LB. Logical analysis in roentgen diagnosis. Radiology 1960;74:178-93. [Crossref] [PubMed]
- Miller DD, Brown EW. Artificial Intelligence in Medical Practice: The Question to the Answer? Am J Med 2018;131:129-33. [Crossref] [PubMed]
- Gehlbach PL. Robotic surgery for the eye. Nat Biomed Eng 2018;2:627-8. [Crossref] [PubMed]
- Briganti G, Le Moine O. Artificial Intelligence in Medicine: Today and Tomorrow. Front Med (Lausanne) 2020;7:27. [Crossref] [PubMed]
- Ajdari A, Liao Z, Mohan R, et al. Personalized mid-course FDG-PET based adaptive treatment planning for non-small cell lung cancer using machine learning and optimization. Phys Med Biol 2022; [Crossref] [PubMed]
- Menni C, Valdes AM, Freidin MB, et al. Real-time tracking of self-reported symptoms to predict potential COVID-19. Nat Med 2020;26:1037-40. [Crossref] [PubMed]
- Romiti S, Vinciguerra M, Saade W, et al. Artificial Intelligence (AI) and Cardiovascular Diseases: An Unexpected Alliance. Cardiol Res Pract 2020;2020:4972346. [Crossref] [PubMed]
- Yu KH, Beam AL, Kohane IS. Artificial intelligence in healthcare. Nat Biomed Eng 2018;2:719-31. [Crossref] [PubMed]
- Murdoch TB, Detsky AS. The inevitable application of big data to health care. JAMA 2013;309:1351-2. [Crossref] [PubMed]
- Sotirakos S, Fouda B, Mohamed Razif NA, et al. Harnessing artificial intelligence in cardiac rehabilitation, a systematic review. Future Cardiol 2022;18:154-64. [Crossref] [PubMed]
- Trezzini B, Meyer B, Ivankovic M, et al. Der administrative Aufwand der Ärzteschaft nimmt weiter zu. Schweizerische Ärztezeitung 2020; [Crossref]
- Coiera E, Kocaballi B, Halamka J, et al. The digital scribe. NPJ Digit Med 2018;1:58. [Crossref] [PubMed]
- FMH. Digital Trends Survey 2021. Available online: www.fmh.ch/digital-trends-survey-2021-fr
- Maskara R, Bhootra V, Thakkar D, et al. A study on the perception of medical professionals towards artificial intelligence. International Journal of Multidisciplinary Research and Development 2017;4:34-9.
- Oh S, Kim JH, Choi SW, et al. Physician Confidence in Artificial Intelligence: An Online Mobile Survey. J Med Internet Res 2019;21:e12422. [Crossref] [PubMed]
- Abdullah R, Fakieh B. Health Care Employees' Perceptions of the Use of Artificial Intelligence Applications: Survey Study. J Med Internet Res 2020;22:e17620. [Crossref] [PubMed]
- Gerke S, Minssen T, Cohen G. Ethical and legal challenges of artificial intelligence-driven healthcare. Artificial Intelligence in Healthcare 2020:295-336.
- Available online: https://datareportal.com/
- Available online: https://saudigazette.com.sa/
- Available online: https://www.vision2030.gov.sa/en/
- Al-Jehani NB, Hawsawi ZA, Radwan N, et al. Development of artificial intelligence techniques in Saudi Arabia: The impact on COVID-19 pandemic. Literature review. Journal of Engineering Science and Technology 2021;16:4530-47.
- Alqahtani A. A Review of the Scope, Future, and Effectiveness of Using Artificial Intelligence in Cardiac Rehabilitation: A Call to Action for the Kingdom of Saudi Arabia. Applied Artificial Intelligence 2023; [Crossref]
- Cabitza F, Rasoini R, Gensini GF. Unintended Consequences of Machine Learning in Medicine. JAMA 2017;318:517-8. [Crossref] [PubMed]
- Karches KE. Against the iDoctor: why artificial intelligence should not replace physician judgment. Theor Med Bioeth 2018;39:91-110. [Crossref] [PubMed]
Cite this article as: Chaieb S, Garrouch K, Al-Ali NS. Perceptions of the use and benefits of artificial intelligence applications: survey study. J Med Artif Intell 2023;6:28.