Artificial intelligence in periodontology and implantology—a narrative review
Introduction
Artificial intelligence (AI) is justifiably one of the most popular buzzwords in technology at present that is revolutionizing all facets of human existence (1). AI is the process of teaching a computer, a computer-controlled robot, or software to think intelligently in the same way that humans do. AI is achieved by examining the characteristics of the human brain and by assessing the cognitive process, leading to the development of intelligent technology (2). AI is defined as “the branch of science and engineering associated with computational knowledge which is commonly referred to as intelligent behavior, as well as the development of systems exhibiting similar behavior”. Artificial intelligent systems are programs that allow computers to function in ways that seem intelligent. Alan Turing [1950], a British mathematician, was one of the pioneers of AI. The term ‘Turing test’, was named after him, which is explained as a computer’s intelligent behavior and its ability to accomplish cognitive tasks on par with humans (3).
The main subdivisions of AI include deep learning (DL), machine learning (ML), robotics, and artificial neural networks (ANNs). AI works in two phases, i.e., a training and a testing phase. The characteristics, associations, and patterns in the data are taught to the AI model in the training phase. Teaching the model to make correct decisions or predictions is the objective of the training phase. The trained AI model makes decisions or predictions for fresh data during the testing phase which were not given during the training phase (4).
AI in dentistry is a fast-expanding field that primarily aims to help dentists provide excellent care to patients by streamlining procedures and saving time (5). AI is revolutionizing dentistry by enabling more precision, reduced errors, and a reduction in staffing needs. It can carry out several tasks in a dental clinic, such as appointment scheduling, and helping with the formulation of a clinical diagnosis and treatment plan (6). AI-based tools aid in enhancing the quality of healthcare at reduced costs for a wider population, and ultimately create the way for personalized, participatory, predictive, and preventive dentistry. Any application of AI in dentistry should show quantifiable benefits, such as improving patient empowerment and support, enhancing accessibility and quality of care, boosting efficiency and safety of services, expanding medical research, or promoting sustainability (7).
In orthodontics, AI has shown good, sensitivity, specificity, precision, and accuracy in the detection and classification of malocclusion. Neural networks can help in the diagnosis and treatment planning, marking of cephalometric points, evaluating the anatomy, analyzing growth and development, predicting the need for orthodontic extraction, and assessing treatment results (5,6). AI can also assist in orthodontic practice, including clinical documentation, remote care, and practice guidance (8).
ANN has been used to assess the risk of oral cancer (5). An AI-enabled system has been used to assist dentists in differentiating between temporomandibular joint (TMJ) disorders by converting chief complaints and history of TMJ disorders into computer language (5).
AI can detect caries and restorations, and help in choosing a suitable method for caries excavation in the field of restorative dentistry (6). In endodontics, neural networks can be used to identify root fractures and periapical lesions, assess the root canal system and the viability of dental pulp stem cells, measure the working length, and predict the prognosis for retreatment procedures (6). Diagnocat (Diagnocat Ltd., San Francisco, CA, USA), an AI-based tool has been used favorably to diagnose periapical periodontitis on periapical radiographs (9).
AI can aid in the treatment planning of orthognathic surgery and dental implants, identify bone lesions, and predict the possibility of complications after extraction. According to a recent systematic review, AI models have considerable potential for identifying implant types, predicting the success of implant treatment, and optimizing the implant design (10).
Bernauer et al. reported that the latest innovations in AI highlight its use in prosthodontics as a tool for diagnosis, identification, classification, and predictive measures (11). AI is also used in pediatric dentistry to assist clinicians in making appropriate diagnoses, clinical decisions, preventive measures, and effective treatment planning (6).
AI is still in its infancy and is not yet fully applied in periodontology. Its advantages in diagnosis and data analysis indicate that there is a lot to gain by using this tool. However, there is insufficient evidence to comprehensively summarize the applications of AI in periodontology. This article aims to review the applications of AI across various facets of periodontal diagnosis and treatment planning, along with its advantages and drawbacks. We present this article in accordance with the Narrative Review reporting checklist (available at https://jmai.amegroups.com/article/view/10.21037/jmai-23-186/rc).
Methods
A comprehensive search was carried out utilizing the databases such as Google Scholar, PubMed, MEDLINE, and Embase, using the keywords “Periodontics AND AI”, “Periodontology AND Artificial Intelligence”, “Periodontology AND neural networks”, and “AI AND periodontal diseases and periodontal therapy” (Table 1). The publication period was set to 20 years. Original articles, clinical trials, and systematic reviews utilizing AI for periodontal diagnosis and treatment, and study designs in which AI was used as the independent variable were included in this review. Studies that were not published in English language, studies which used other software rather than AI-based tools, and studies which used AI for purposes other than periodontology and implantology were excluded.
Table 1
| Items | Specification |
|---|---|
| Date of search | 25 September 2023, 25 November 2023 |
| Databases and other sources searched | Google Scholar, PubMed, MEDLINE, and Embase |
| Search terms used | “Periodontics AND AI”, “Periodontology AND Artificial Intelligence”, “Periodontology AND neural networks”, and “AI AND periodontal diseases and periodontal therapy” |
| Timeframe | 2003–2023 |
| Inclusion and exclusion criteria | Inclusion criteria: original articles, clinical trials, and systematic reviews utilizing AI for periodontal diagnosis and treatment, and study designs in which AI was used as the independent variable |
| Exclusion criteria: studies that were not published in English language, studies which used other software rather than AI-based tools, and studies which used AI for purposes other than periodontology and implantology | |
| Selection process | Conducted independently by first author, consensus was obtained after reviewing the full texts |
AI, artificial intelligence.
A single reviewer screened titles and abstracts. After a detailed review of the abstracts, the most relevant papers related to our topic were included, and any irrelevant articles were excluded. Full texts were reviewed by all the authors to determine their eligibility for studies which met the inclusion criteria, or where there was uncertainty to obtain consensus. Data was extracted from the studies and recorded in a tabulated form. The standardized data collation included the author names, year of publication, and the applications of AI.
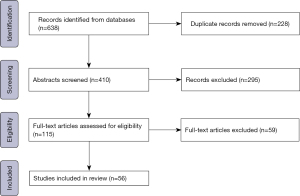
The study selection process is outlined in Figure 1. A total of 410 articles were identified for screening. In total, 295 texts were excluded after screening for factors not meeting inclusion criteria. Full-text review identified 56 studies for inclusion in the review.
AI in periodontology
The amount of research on the use of AI models in periodontics has been growing exponentially, which has shown that in the future years, AI will transform periodontology with its various techniques and applications (12). AI can assist in the timely diagnosis of periodontitis by evaluating radiographs and detecting changes in the periodontium, which permits quick intervention and improved treatment results.
Detection of periodontal disease
Intraoral photos and microscopic images of dental plaque have been analyzed by AI-based systems for the detection of periodontal disease (Table 2). Good reliability and accuracy have been reported with the use of AI models to assess bone loss and diagnose periodontal disease.
Table 2
| Author, year | Study | Findings |
|---|---|---|
| Lee et al., 2018 (13) | Deep CNN-based computer-assisted detection system in the diagnosis and prediction of PCT | PCT were diagnosed with an accuracy of 76.7% for molars and 81% for premolars. Extraction was predicted with an accuracy of 73.4% for molars and 82.8% for premolars in severely compromised teeth. The diagnosis and prediction of PCT was successfully performed using the deep CNN algorithm |
| Aberin et al., 2018 (14) | Differentiation between periodontitis-affected and healthy dental plaque using microscopic images of dental plaque and the AlexNet architectural model based on CNNs | The model showed an accuracy of 75.5% and a mean square error of 0.05348436995 |
| Balaei et al., 2017 (15) | Detection of periodontitis for people with limited access to dental personnel and facilities in any healthcare setting considering pretreatment intraoral photos as diseased individuals, and the posttreatment photos as healthy individuals | Pre- and post-treatment have been classified as healthy or diseased individuals with an accuracy of 91.6%. The algorithm is useful as a smartphone application for people with limited access to dental clinics to be screened for periodontitis by health professionals in any healthcare setting, and to monitor the progress of periodontal treatment |
AI, artificial intelligence; CNN, convolutional neural network; PCT, periodontally compromised teeth.
Classification of periodontal diseases
AI models have been used to classify periodontal disease, differentiate between chronic and aggressive periodontitis, and distinguish healthy from inflamed gingival (Table 3). AI models have been observed to have a potentially effective and significant ability to identify differences, classify, and identify diseases.
Table 3
| Author, year | Study | Findings |
|---|---|---|
| Feres et al., 2018 (16) | Classification of patients into generalized ChP, generalized AgP, and PH by ML using 40 bacterial species | A support vector classifier using a panel of 40 bacterial species was useful to differentiate between PH, ChP, and AgP. The relative bacterial load could distinguish between AgP and ChP |
| Rana et al., 2017 (17) | A ML classifier trained with annotations from dentists that gives pixel-wise inflammation segmentations of color-augmented intraoral photos | The classifier differentiates successfully between healthy and inflamed gingiva with precision and recall of 0.347 and 0.621, respectively. The early diagnosis of periodontal diseases given by this classifier using photos acquired by intraoral imaging devices can be advantageous for dentists and patients |
| Ozden et al., 2015 (18) | Classification of periodontal diseases using ANNs, SVM, and DT | DT and SVM showed the best accuracy of 98% in the classification of periodontal diseases with a computational time of 19.91 and 7.00 s, respectively. SVM and DT are simple enough to comprehend; they reflect all the factors associated with periodontal status and are useful as a tool for decision-making and prediction of periodontal disease |
AI, artificial intelligence; ChP, chronic periodontitis; AgP, aggressive periodontitis; PH, periodontal health; ML, machine learning; ANN, artificial neural network; SVM, support vector machine; DT, decision tree.
Periodontal risk assessment (PRA)
AI algorithms for PRA have been developed and compared with previous PRA models, producing reliable predictions (Table 4). These AI algorithms have been found to be simple yet beneficial tools for making decisions when predicting periodontal disease since they were simple to comprehend and took into account a variety of characteristics related to periodontal disease.
Table 4
| Author, year | Study | Findings |
|---|---|---|
| Moosa et al., 2023 (19) | ML model to study the association between patient demographics, smoking, treatment received, and severity of periodontal disease before and after treatment | The ML model, random forest regressor, showed less potential for prediction of post-treatment severity. However, it can reflect the associations between patient demographics and disease-specific factors in periodontal disease |
| Patel et al., 2022 (20) | Comparison of patient’s risk factors in five PRA tools (PRA, PreViser, Sonicare, Cigna, and PRSS developed using ML) | The most precise prediction was given by PRSS (70%), followed by Previser (55%), PRA (35%), Phillips (35%), and Cigna (25%) |
| Yauney et al., 2019 (21) | Correlation of periodontal disease with systemic health conditions using a combination of ML, clinical examination, and intraoral fluorescent porphyrin biomarker imaging | The results indicate a positive correlation between systemic health conditions and poor periodontal health. The screening analysis method using ML and images can be used for diagnoses and screening of other systemic diseases |
| Shankarapillai et al., 2010 (22) | Prediction of periodontal risk using two ANN algorithms namely: Levenberg Marquardt and Scaled Conjugate Gradient algorithms | The Levenberg Marquardt algorithm outperformed the Scaled Conjugate Gradient algorithm with fewer repetitions, faster convergence, and producing the smallest mean square error in both the training and testing phases. Levenberg Marquardt algorithm can effectively be used as a well-trained neural network for the prediction of the risk for periodontitis |
AI, artificial intelligence; PRA, periodontal risk assessment; ML, machine learning; PRSS, Periodontal Risk Scoring System; ANN, artificial neural network.
Assessment of periodontal bone level
Calculation of radiographic bone loss (RBL) can be complicated, time-consuming, and subjective to the examiner. Hence, AI algorithms have been created to automatically identify RBL and the likelihood of tooth loss and periodontal disease (Table 5). Miller et al. [2023] reviewed the potential of AI models to detect RBL for the diagnosis of periodontal disease. They observed that the mean accuracy in the case of panoramic radiographs ranged between 63% and 94%, while periapical radiographs showed a precision of 25% for detecting mild disease and a high accuracy of 99% for staging of RBL. Specificity for periodontal bone loss ranged between 81% and 83% on cone-beam computed tomography (CBCT), while sensitivity was 45–72% (26). AI systems can be a good starting point for screening radiographs for periodontal disease. AI models created for the detection of RBL and periodontal disease require further refinement to effectively and consistently evaluate RBL and calculate the periodontal disease risk without the need for assessment by a clinician.
Table 5
| Author, year | Study | Findings |
|---|---|---|
| Alotaibi et al., 2022 (23) | Detection of alveolar bone loss and classification of the severity of bone loss due to periodontal disease in periapical radiographs in the anterior region of the dental arches using a computer-assisted detection system based on a deep CNN algorithm | Alveolar bone loss was detected with an accuracy of 73%, and the accuracy of classification of the level of severity of the bone loss was 59%. Alveolar bone loss was effectively detected in periapical radiographs using the deep CNN algorithm (VGG-16). Also, the severity of bone loss was detected satisfactorily. Periodontal disease can be detected and staged efficiently using a computer-aided CNN algorithm-based detection system |
| Chang et al., 2020 (24) | DL hybrid method for the diagnosis of periodontal bone loss and staging of periodontitis on dental panoramic radiographs | Diagnosis and staging of periodontitis were performed with good reliability and excellent accuracy using the combination of DL and the conventional CAD method |
| Krois et al., 2019 (25) | Detection of PBL on panoramic radiographs using deep CNNs | The mean accuracy for classification by CNN was 0.81, and that of the dentists was 0.76. There was no statistically significant difference between CNN and the examiners. The CNN showed comparable ability as dentists in the detection of PBL on panoramic radiographs. Technologies based on ML may help reduce the dentist’s efforts |
AI, artificial intelligence; CNN, convolutional neural network; DL, deep learning; CAD, computer-aided design; PBL, periodontal bone loss; ML, machine learning.
Artificial olfaction for detection of halitosis
An array of non-selective sensors is used to evaluate the total spectrum of exhaled volatile compounds for artificial olfaction. It is also called an electronic nose as it is a combination of mammalian olfaction and AI which identifies specific patterns of smell and is used as a reference for future identification. The programmed sensor array consists of two subsets in which the bottom panel has a higher affinity for volatile sulfur compounds (VSCs), and the top panel has a higher affinity for non-sulfuric volatile organic compounds. On exposure to the sample, the sensors react simultaneously and the responses are processed for pattern recognition. The software compares the patterns obtained from different sensors with the database of patterns previously obtained during the phases of preclinical training. A decision tree-based classifier determines if a subject has oral or extraoral halitosis. It will also classify the volatolomic pattern based on different systemic diseases in the case of extraoral halitosis (27). Nakhleh et al. [2017] demonstrated an AI-based sensor array consisting of 20 functionalized nanomaterials-based sensors that could successfully differentiate between 17 systemic diseases by analyzing the exhaled breath with 86% accuracy (28).
AI in implantology
Implant dentistry has undergone a paradigm shift with the use of AI technology. AI algorithms reduce risks, optimize aesthetics, and improve the accuracy of implant placement. AI-based data analysis improves success rates by providing significant insights into treatment plans that are also patient-specific.
Treatment planning
CBCT scans are the radiographic method of choice for planning dental implant treatments throughout the world. AI can be helpful for clinicians who face difficulties in evaluating CBCT scans for thorough implant planning and recognition of anatomical structures. Three-dimensional (3D) dental implant placement is essential in the current scenario of prosthetically driven implantology. AI assists dental practitioners in the decision-making process and can be an asset to dental implant planning (Table 6).
Table 6
| Author, year | Application of AI in implantology | Findings |
|---|---|---|
| Moufti et al., 2023 (29) | Identify and demarcate edentulous alveolar bone on CBCT images before implant placement | ML showed better accuracy in the segmentation of the edentulous alveolar bone on CBCT images as compared to manual segmentation |
| Fontenele et al., 2023 (30) | CNN-based tool for automated segmentation of 3D maxillary alveolar bone on CBCT images | The CNN-based tool provided an accurate segmentation of the maxillary alveolar bone and its crestal contour, which was comparable with the manual segmentation. The AI-based segmentation (51.5±10.9 s) was 116 times faster than manual segmentation |
| Oliveira-Santos et al., 2023 (31) | Segmentation of mandibular canal using an AI-based tool in the presence of anatomical variation like the anterior loop | Segmentation of the mandibular canal was achieved accurately even in the presence of an anterior loop |
| Mangano et al., 2023 (32) | AI and AR for 3D dental implant planning | The new protocol is time-efficient and effective for planning simple static-guided implant treatment cases in partially edentulous patients. The accuracy of implant placement was acceptable. Conventional software may be replaced by AI and AR technologies for 3D implant planning and guided implant surgery |
| Sakai et al., 2023 (33) | Determination of a suitable protocol for implant drilling using CBCT images | The drilling protocol was effectively predicted from CBCT images by the AI model. A decision-making support system based on AI can be developed to improve primary stability |
| Morgan et al., 2022 (34) | Segmentation of maxillary sinus from CBCT images using an automated CNN-based model | The CNN model allows a precise generation of 3D models for diagnosis and virtual treatment planning by providing a time-efficient, accurate, and reliable segmentation |
| Kurt Bayrakdar et al., 2021 (35) | AI system in implant planning using 3D CBCT images | No statistically significant differences in the bone height measurements between AI and manual measurements. There were statistically significant differences between AI and manual measurements in the bone thickness measurements. Also, the detection accuracy was 72.2% for canals, 66.4% for sinuses/fossae, and 95.3% for missing tooth regions |
| Kwak et al., 2020 (36) | Identification and segmentation of mandibular canal on CBCT images using DL networks | The deep CNN model was successfully used for the detection of the mandibular canal |
AI, artificial intelligence; CBCT, cone-beam computed tomography; ML, machine learning; CNN, convolutional neural network; 3D, three-dimensional; AR, augmented reality; DL, deep learning.
Detection of implant type
Numerous implant brands are available throughout the world with prosthetic components and different abutments. Additional surgical, periodontal, or prosthetic procedures may be necessary if any complications occur with the implants or their components, and more information, including the implant length, diameter, platform, manufacturer and abutment type will be required during such events. If the implant treatment was provided at a different clinic and if the treatment provider cannot be contacted, it can be cumbersome to obtain the information. The use of AI for the detection of the implant brand can be a solution to this problem (Table 7).
Table 7
| Author, year | Application of AI in implantology | Findings |
|---|---|---|
| Park et al., 2023 (37) | Automated identification and classification of different DISs using DL algorithm | The automated DL demonstrated a reliable accuracy of 88.53% for classification based on 40,209 periapical and 116,756 panoramic radiographs |
| da Mata Santos et al., 2021 (38) | AI-based computer-assisted system for the identification of implant brands using periapical radiographs | The CNN is of good clinical significance which identified implant manufacturers precisely with an accuracy of 85.29% |
| Benakatti et al., 2021 (39) | Detection of implant systems from panoramic radiographs using ML | Implant systems can be identified proficiently using the tested ML models, i.e., logistic regression, support vector machine, X boost classifiers, and K Nearest neighbor |
| Takahashi et al., 2020 (40) | The DL model for the identification of implant systems | DL models can be used to identify implant systems from panoramic radiographs, which can be helpful for clinicians and patients as well. The training of these models can be improved by adding images of more implant systems for their clinical application |
| Lee et al., 2020 (41) | Automated classification of DISs using DCNN | The automated DCNN was very efficient in classifying various types of DISs from dental radiographs, and it could outperform most specialists |
| Sukegawa et al., 2020 (42) | Classification of different dental implant brands from panoramic radiographs using deep CNNs | 11 types of panoramic radiographs were accurately classified by the VGG-19 and VGG-16 CNNs |
AI, artificial intelligence; DIS, dental implant system; DL, deep learning; CNN, convolutional neural network; ML, machine learning; DCNN, deep convolutional neural network.
Chaurasia et al. [2024] reported an accuracy of 70.75% to 98.19% for the identification and classification of different implant systems (DISs) from periapical and panoramic radiographs using DL models amongst nine studies included in their systematic review and meta-analysis (43). A systematic review by Revilla-León et al. [2023] found that the AI models created to identify the type of implant using radiographs showed an accuracy of 93.8–98%, and is a more advanced application of AI in implantology (10).
Optimization of implant designs
AI algorithms have been used in tandem with finite element analysis (FEA) to optimize implant designs (Table 8). In a systematic review by Revilla-León et al. [2023], it was concluded that the AI models can be used to minimize stress at the implant-bone interface by 36.6% when compared to FEA models, optimize the implant design, length, diameter, and porosity, and enhance FEA calculations, or precisely determine the elastic modulus of the implant-bone interface (10).
Table 8
| Author, year | Application of AI in implantology | Findings |
|---|---|---|
| Li et al., 2019 (44) | Reduction of the stress at the implant-bone interface by optimization approach for dental implants | Implant optimization by support vector regression is reliable and efficient and can replace the finite element method |
| Roy et al., 2018 (45) | Utilizing ANNs, FEA, genetic algorithms, and desirability functions in conjunction to design the morphology of dental implants to produce the appropriate microstrain | A genetic algorithm can be used successfully to design a dental implant and obtain the appropriate implant stress and microstrain. ANN model is a good method of optimization to convert the findings of FEA, with reduced computational expenses |
| Zaw et al., 2009 (46) | Identify Young’s elastic modulus of the tissue between a dental implant and bone using the NN and RBM based rapid inverse analysis method | The RBM-NN method was accurate, efficient, and reliable for inverse material characterizations in noninvasive and/or nondestructive evaluations, with significantly lower computational costs |
AI, artificial intelligence; ANN, artificial neural network; FEA, finite element analysis; NN, neural network; RBM, reduced-basis method.
Prediction of treatment outcomes
Complications of implant treatment continue to rise with dental implants being the most preferred treatment modality for patients as well as clinicians. These complications are responsible for added procedures and greater treatment costs. Accurate prediction of the therapeutic outcome in implant dentistry is necessary and AI is expected to play a significant role in this area. Neural networks have been used in previous studies to predict the risk of loss of an implant (Table 9). The accuracy of AI algorithms ranged from 62.4% to 80.5% in predicting the success of an implant or osseointegration in a systematic review by Revilla-León et al. [2023] (10).
Table 9
| Author, year | Application of AI in implantology | Findings |
|---|---|---|
| Zhang et al., 2023 (47) | Prediction of implant outcome using periapical and panoramic radiographs | Implant failures were predicted with an accuracy of 87% from periapical and panoramic radiographs using the DL model, which can be helpful to begin clinical intervention at early stages |
| Oh et al., 2023 (48) | DL-based prediction of osseointegration of dental implants using plain radiography | Prediction of dental implant osseointegration showed an accuracy of approximately 4/5 |
| Lyakhov et al., 2022 (49) | Prediction of the success of a single implant by analyzing patient statistics using an AI system | The AI system showed 94.48% accuracy in the detection of patient statistics to predict the success of single implants. This system can improve implant survival and minimize complications by highlighting the less significant patient factors that affect the quality of the implant installation |
| Huang et al., 2022 (50) | Prediction of the risk of loss of dental implants using DL based on preoperative CBCT | The IM (created by a combination of clinical features with DL) can assist clinicians in evaluating preoperative risks as it successfully predicts the risk of loss of an implant within 5 years |
AI, artificial intelligence; DL, deep learning; CBCT, cone-beam computed tomography; IM, integrated model.
Chat-generative pre-trained transformer (ChatGPT) in periodontology
ChatGPT is an AI program that generates responses that resemble those of a human using DL techniques. Its ability to handle a wide range of topics as a dynamic conversational agent makes it valuable for chatbots, customer support, and other applications. ChatGPT has a multitude of applications in dentistry which include providing telemedicine services for dentistry, aiding in the clinical judgments made by the dentist, enhancing the education of dental students, and helping with the composition of patient information, scientific evaluations, and articles (Table 10) (51,52).
Table 10
| Author, year | Application of AI in implantology | Findings |
|---|---|---|
| Babayiğit et al., 2023 (51) | Evaluation of the accuracy and completeness of the answers to the most frequently asked questions on various topics in periodontology by ChatGPT | With regards to accuracy, ChatGPT’s answers to the most frequently asked questions by patients in periodontology were “nearly completely correct”, and “adequate” with regards to completeness |
| Alan et al., 2023 (52) | Evaluation of the quality of information produced by ChatGPT-4 on PD | It can be regarded as being helpful for PD patients looking for information, despite certain limitations in giving comprehensive information on treatment choice, as it consistently provided accurate information in most of the responses |
ChatGPT, chat-generative pre-trained transformer; AI, artificial intelligence; PD, periodontal disease.
Periodontists can use ChatGPT as an informative tool, even though it may not provide perfect accuracy and thorough results without professional supervision. Nevertheless, it must be highlighted that errors may occur.
AI in dental practice
Appointment scheduling is one area where AI is revolutionizing dental practice administration. AI models evaluate several variables, including patient preferences, dentist availability, and treatment durations, to automatically plan appointments in a way that maximizes effectiveness and minimizes disputes. This saves clinicians’ time and improves patient satisfaction by ensuring seamless appointment experiences and shorter wait times (53).
The ability of AI to track and optimize patient visits to preemptively schedule incomplete treatment and launch new-patient marketing campaigns based on profit maximization algorithms is another sophisticated feature of appointment scheduling. ML algorithms that can communicate with dental office software enable this kind of optimization (54).
In terms of general inquiries from patients, all the easy questions can be handled easily by AI. DL algorithms allow for the search of patient records to find the most profitable patient therapy. As a result, assistants can respond more quickly in the event of a patient emergency before the scheduled appointment and spend less time managing prescriptions after surgery. Furthermore, AI can assist the dental practitioner concerning the patient’s allergies and any pertinent medical history. AI can also be used by patients participating in tobacco or smoking cessation programs, to schedule important reminders (54).
In contrast to the conventional techniques in dental practices, AI software enables us to create a thorough virtual database for every patient that is simultaneously accessible and user-friendly. Any dental intervention gains reliability because the AI software can acquire all required data from the database more quickly and efficiently than a human (e.g., collection of dental records, radiographs, and extraoral photographs, essential for diagnosis). The AI system’s exceptional capacity for learning allows it to be “trained” to carry out a wide range of additional tasks. It can be combined, for example, with imaging techniques such as CBCT and magnetic resonance imaging (MRI) to detect minute variations from normalcy that could have not been noticed otherwise. If seen as a complementary tool, AI can aid with a variety of dental procedures or enhance awareness of periodontal diseases, urging patients to seek timely treatment (54).
Urban et al. [2023] reviewed the potential effects of AI support on CBCT data processing in dental clinics and its effects on the transformation of the roles of nurses and dental assistants in the future (55). AI can be used in the following ways for the management of CBCT data:
- AI models can be trained to process and analyze CBCT images for any specific dental condition;
- A comprehensive overview of the patient’s oral health can be obtained by integrating CBCT data with other patient information, such as electronic dental records and intraoral scans;
- AI tools can aid nurses and dental assistants in communicating the CBCT data clearly to patients, assisting them to better comprehend their oral health and treatment options;
- AI models can be used to identify distortions or artifacts that can affect the interpretation of images to ensure good quality of CBCT images.
Advantages of AI
- Gives accurate and updated information;
- Streamlines automated tasks such as scheduling appointments, patient tracking, obtaining clinical data, and treatment guidance for patients;
- Saves time and resources by automating essential procedures, as a result of which clinicians have more time to examine patients and identify diseases;
- Assists in research by gathering vast amounts of information from several sources (56).
Disadvantages of AI
- Needs human surveillance as AI operates with logical reasoning and not with empathy;
- May overlook social variables such as economic, social, and historical issues;
- May lead to unemployment and equity concerns could arise from this variable if it causes professionals to lose their jobs after spending money and effort on healthcare education;
- Inaccuracies are still possible when there is limited data on specific diseases, environmental factors, or demographics;
- Privacy concerns may arise while using AI as several multinational companies are unrestricted in their ability to gather and utilize data (56).
Conclusions
AI can improve the effectiveness of periodontists as decision aids and decision-making tools. To gain widespread implementation, AI systems must receive regulatory approval, incorporation with public healthcare systems, standardization for reliable operation, clinical advice and training, and appropriate financing for continuous operation. However, it must be highlighted that AI cannot replace clinicians; instead, they can support periodontists as they provide patient care, with clinicians adopting roles that best utilize special human skills like compassion, motivation, and comprehensive assimilation as part of a holistic patient-centric healthcare system.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the Narrative Review reporting checklist. Available at https://jmai.amegroups.com/article/view/10.21037/jmai-23-186/rc
Peer Review File: Available at https://jmai.amegroups.com/article/view/10.21037/jmai-23-186/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jmai.amegroups.com/article/view/10.21037/jmai-23-186/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Artificial intelligence. 2023. Accessed: December 6, 2023. Available online: https://www.oecd.org/digital/artificial-intelligence/
- Duggal N. What is Artificial Intelligence and Why It Matters in 2024? 2023. Accessed: December 6, 2023. Available online: https://www.simplilearn.com/tutorials/artificial-intelligence-tutorial/what-is-artificial-intelligence
- Ramesh AN, Kambhampati C, Monson JR, et al. Artificial intelligence in medicine. Ann R Coll Surg Engl 2004;86:334-8. [Crossref] [PubMed]
- Altalhi AM, Alharbi FS, Alhodaithy MA, et al. The Impact of Artificial Intelligence on Dental Implantology: A Narrative Review. Cureus 2023;15:e47941. [Crossref] [PubMed]
- Ramani S, Vijayalakshmi R, Mahendra J, et al. Artificial intelligence in periodontics-An overview. IP Int J Periodontol Implantol 2023;8:71-4. [Crossref]
- Alhaidry HM, Fatani B, Alrayes JO, et al. ChatGPT in Dentistry: A Comprehensive Review. Cureus 2023;15:e38317. [PubMed]
- Schwendicke F, Samek W, Krois J. Artificial Intelligence in Dentistry: Chances and Challenges. J Dent Res 2020;99:769-74. [Crossref] [PubMed]
- Liu J, Zhang C, Shan Z. Application of Artificial Intelligence in Orthodontics: Current State and Future Perspectives. Healthcare (Basel) 2023.
- Issa J, Jaber M, Rifai I, et al. Diagnostic Test Accuracy of Artificial Intelligence in Detecting Periapical Periodontitis on Two-Dimensional Radiographs: A Retrospective Study and Literature Review. Medicina (Kaunas) 2023;59:768. [Crossref] [PubMed]
- Revilla-León M, Gómez-Polo M, Vyas S, et al. Artificial intelligence applications in implant dentistry: A systematic review. J Prosthet Dent 2023;129:293-300. [Crossref] [PubMed]
- Bernauer SA, Zitzmann NU, Joda T. The Use and Performance of Artificial Intelligence in Prosthodontics: A Systematic Review. Sensors (Basel) 2021;21:6628. [Crossref] [PubMed]
- Shirmohammadi A, Ghertasi Oskouei S. The growing footprint of artificial intelligence in periodontology & implant dentistry. J Adv Periodontol Implant Dent 2023;15:1-2. [Crossref] [PubMed]
- Lee JH, Kim DH, Jeong SN, et al. Diagnosis and prediction of periodontally compromised teeth using a deep learning-based convolutional neural network algorithm. J Periodontal Implant Sci 2018;48:114-23. [Crossref] [PubMed]
- Aberin STA, de Goma JC. Detecting periodontal disease using convolutional neural networks. 2018 IEEE 10th International Conference on Humanoid, Nanotechnology, Information Technology, Communication and Control, Environment and Management (HNICEM). IEEE; 2018:1-6.
- Balaei AT, de Chazal P, Eberhard J, et al. Automatic detection of periodontitis using intra-oral images. Annu Int Conf IEEE Eng Med Biol Soc 2017;2017:3906-9. [PubMed]
- Feres M, Louzoun Y, Haber S, et al. Support vector machine-based differentiation between aggressive and chronic periodontitis using microbial profiles. Int Dent J 2018;68:39-46. [Crossref] [PubMed]
- Rana A, Yauney G, Wong LC, et al. Automated segmentation of gingival diseases from oral images. 2017 IEEE Healthcare Innovations and Point of Care Technologies (HI-POCT). IEEE; 2017:144-7.
- Ozden FO, Özgönenel O, Özden B, et al. Diagnosis of periodontal diseases using different classification algorithms: a preliminary study. Niger J Clin Pract 2015;18:416-21. [Crossref] [PubMed]
- Moosa Y, Bacha SH, Raza SA, et al. Role of Artificial Intelligence in Periodontology. Pakistan Journal of Medical & Health Sciences 2023;17:363-8. [Crossref]
- Patel JS, Patel K, Vo H, et al. Enhancing an AI-Empowered Periodontal CDSS and Comparing with Traditional Perio-risk Assessment Tools. AMIA Annu Symp Proc 2022;2022:846-55. [PubMed]
- Yauney G, Rana A, Wong LC, et al. Automated process incorporating machine learning segmentation and correlation of oral diseases with systemic health. 2019 41st Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC). IEEE; 2019:3387-93.
- Shankarapillai R, Mathur LK, Nair MA, et al. Periodontitis risk assessment using two artificial neural networks-a pilot study. Int J Dent Clin 2010;2:36-40.
- Alotaibi G, Awawdeh M, Farook FF, et al. Artificial intelligence (AI) diagnostic tools: utilizing a convolutional neural network (CNN) to assess periodontal bone level radiographically-a retrospective study. BMC Oral Health 2022;22:399. [Crossref] [PubMed]
- Chang HJ, Lee SJ, Yong TH, et al. Deep Learning Hybrid Method to Automatically Diagnose Periodontal Bone Loss and Stage Periodontitis. Sci Rep 2020;10:7531. [Crossref] [PubMed]
- Krois J, Ekert T, Meinhold L, et al. Deep Learning for the Radiographic Detection of Periodontal Bone Loss. Sci Rep 2019;9:8495. [Crossref] [PubMed]
- Miller A, Huang C, Brody ER, et al. CE Credit. Artificial Intelligence Applications for the Radiographic Detection of Periodontal Disease: A Scoping Review. J Calif Dent Assoc 2023;51:2206301. [Crossref]
- Nakhleh MK, Quatredeniers M, Haick H. Detection of halitosis in breath: Between the past, present, and future. Oral Dis 2018;24:685-95. [Crossref] [PubMed]
- Nakhleh MK, Amal H, Jeries R, et al. Diagnosis and Classification of 17 Diseases from 1404 Subjects via Pattern Analysis of Exhaled Molecules. ACS Nano 2017;11:112-25. [Crossref] [PubMed]
- Moufti MA, Trabulsi N, Ghousheh M, et al. Developing an Artificial Intelligence Solution to Autosegment the Edentulous Mandibular Bone for Implant Planning. Eur J Dent 2023;17:1330-7. [Crossref] [PubMed]
- Fontenele RC, Gerhardt MDN, Picoli FF, et al. Convolutional neural network-based automated maxillary alveolar bone segmentation on cone-beam computed tomography images. Clin Oral Implants Res 2023;34:565-74. [Crossref] [PubMed]
- Oliveira-Santos N, Jacobs R, Picoli FF, et al. Automated segmentation of the mandibular canal and its anterior loop by deep learning. Sci Rep 2023;13:10819. [Crossref] [PubMed]
- Mangano FG, Admakin O, Lerner H, et al. Artificial intelligence and augmented reality for guided implant surgery planning: A proof of concept. J Dent 2023;133:104485. [Crossref] [PubMed]
- Sakai T, Li H, Shimada T, et al. Development of artificial intelligence model for supporting implant drilling protocol decision making. J Prosthodont Res 2023;67:360-5. [Crossref] [PubMed]
- Morgan N, Van Gerven A, Smolders A, et al. Convolutional neural network for automatic maxillary sinus segmentation on cone-beam computed tomographic images. Sci Rep 2022;12:7523. [Crossref] [PubMed]
- Kurt Bayrakdar S, Orhan K, Bayrakdar IS, et al. A deep learning approach for dental implant planning in cone-beam computed tomography images. BMC Med Imaging 2021;21:86. [Crossref] [PubMed]
- Kwak GH, Kwak EJ, Song JM, et al. Automatic mandibular canal detection using a deep convolutional neural network. Sci Rep 2020;10:5711. [Crossref] [PubMed]
- Park W, Huh JK, Lee JH. Automated deep learning for classification of dental implant radiographs using a large multi-center dataset. Sci Rep 2023;13:4862. [Crossref] [PubMed]
- da Mata Santos RP, Vieira Oliveira Prado HE, Soares Aranha Neto I, et al. Automated Identification of Dental Implants Using Artificial Intelligence. Int J Oral Maxillofac Implants 2021;36:918-23. [Crossref] [PubMed]
- Benakatti VB, Nayakar RP, Anandhalli M. Machine learning for identification of dental implant systems based on shape - A descriptive study. J Indian Prosthodont Soc 2021;21:405-11. [Crossref] [PubMed]
- Takahashi T, Nozaki K, Gonda T, et al. Identification of dental implants using deep learning-pilot study. Int J Implant Dent 2020;6:53. [Crossref] [PubMed]
- Lee JH, Kim YT, Lee JB, et al. A Performance Comparison between Automated Deep Learning and Dental Professionals in Classification of Dental Implant Systems from Dental Imaging: A Multi-Center Study. Diagnostics (Basel) 2020;10:910. [Crossref] [PubMed]
- Sukegawa S, Yoshii K, Hara T, et al. Deep Neural Networks for Dental Implant System Classification. Biomolecules 2020;10:984. [Crossref] [PubMed]
- Chaurasia A, Namachivayam A, Koca-Ünsal RB, et al. Deep-learning performance in identifying and classifying dental implant systems from dental imaging: a systematic review and meta-analysis. J Periodontal Implant Sci 2024;54:3-12. [Crossref] [PubMed]
- Li H, Shi M, Liu X, et al. Uncertainty optimization of dental implant based on finite element method, global sensitivity analysis and support vector regression. Proc Inst Mech Eng H 2019;233:232-43. [Crossref] [PubMed]
- Roy S, Dey S, Khutia N, et al. Design of patient specific dental implant using FE analysis and computational intelligence techniques. Appl Soft Comput 2018;65:272-9. [Crossref]
- Zaw K, Liu GR, Deng B, et al. Rapid identification of elastic modulus of the interface tissue on dental implants surfaces using reduced-basis method and a neural network. J Biomech 2009;42:634-41. [Crossref] [PubMed]
- Zhang C, Fan L, Zhang S, et al. Deep learning based dental implant failure prediction from periapical and panoramic films. Quant Imaging Med Surg 2023;13:935-45. [Crossref] [PubMed]
- Oh S, Kim YJ, Kim J, et al. Deep learning-based prediction of osseointegration for dental implant using plain radiography. BMC Oral Health 2023;23:208. [Crossref] [PubMed]
- Lyakhov PA, Dolgalev AA, Lyakhova UA, et al. Neural network system for analyzing statistical factors of patients for predicting the survival of dental implants. Front Neuroinform 2022;16:1067040. [Crossref] [PubMed]
- Huang N, Liu P, Yan Y, et al. Predicting the risk of dental implant loss using deep learning. J Clin Periodontol 2022;49:872-83. [Crossref] [PubMed]
- Babayiğit O, Tastan Eroglu Z, Ozkan Sen D, et al. Potential Use of ChatGPT for Patient Information in Periodontology: A Descriptive Pilot Study. Cureus 2023;15:e48518. [Crossref] [PubMed]
- Alan R, Alan BM. Utilizing ChatGPT-4 for Providing Information on Periodontal Disease to Patients: A DISCERN Quality Analysis. Cureus 2023;15:e46213. [Crossref] [PubMed]
- How AI will change running a dental practice. 2023. Accessed: December 7, 2023. Available online: https://samera.co.uk/learning-center/how-ai-will-change-running-a-dental-practice/#Streamlining_appointment_scheduling_and_patient_management_with_AI
- Surdilovic D, Ille T, D’Souza J. Artificial intelligence and dental practice management. European Journal of Artificial Intelligence and Machine Learning 2022;1:11-4. [Crossref]
- Urban R, Haluzová S, Strunga M, et al. AI-assisted CBCT data management in modern dental practice: benefits, limitations and innovations. Electronics 2023;12:1710. [Crossref]
- Pros & cons of artificial intelligence in medicine. 2021. Accessed: December 7, 2023. Available online: https://drexel.edu/cci/stories/artificial-intelligence-in-medicine-pros-and-cons/
Cite this article as: Khan SF, Siddique A, Khan AM, Shetty B, Fazal I. Artificial intelligence in periodontology and implantology—a narrative review. J Med Artif Intell 2024;7:6.